Dear Administrator Brooks-LaSure and Deputy Administrator Fowler:
On behalf of the Board of Directors of the Community Oncology Alliance (“COA”), we are asking you to please extend the Oncology Care Model (“OCM”) past the scheduled termination date of June 30, 2022, and to announce this extension immediately.
As you know, the OCM starts winding down on January 1, 2022, with no new patients enrolled past that date. For important reasons summarized in this letter, the OCM should be extended at least through December 31, 2022, while we commit to working with you and the staff at the Center for Medicare and Medicaid Innovation (“CMMI”) to refine and expand the OCM, with a particular emphasis on correcting health disparities in cancer care. The millions of dollars of taxpayers’ money invested in the OCM and the dramatic successes of many independent community oncology practices participating in the OCM in enhancing patient cancer care while lowering treatment costs, should be clear reasons why the OCM should not be trashed, but refined and re-envisioned based on what is working.
We appreciate your recently announced Innovation Center Strategy Refresh.[1] On paper, many of the “refresh” elements are important facets to making CMMI a success, especially the advancement of health equities, and are pertinent to furthering cancer care in this country; however, the reality faced by community oncology practices is that so many are already deeply invested in the OCM in terms of process change, staff, and infrastructure. In fact, it’s ironic that while the OCM has precipitated the remarkable birth of at least 35 oncology payment reform models in this country[2], with many new novel ones under development, the OCM has apparently been deemed a failure by CMMI after just five performance periods, even though it has been a remarkable success in many independent practices.
Many of the current OCM participants have openly and eagerly shared how the OCM has transformed their practices’ mission, teams, and clinical processes to focus on quality and value in all aspects of the cancer care journey. The OCM was instrumental in creating and fostering that mindset. These practice transformations have led to many new initiatives and arrangements with payers to enhance the quality of cancer care while lowering costs. If the OCM is summarily discontinued, especially without a meaningful next-generation model, the clear message will be delivered that the Centers for Medicare & Medicaid Services (“CMS”) and CMMI have no interest in furthering the transformation of the cancer care delivery system in this country. Significantly, it also forfeits CMMI’s leadership role in innovating oncology payment reform.
Recently, Dr. Kashyap Patel presented to CMMI leadership and staff a successor model to the OCM that would focus specifically on health disparities. During the course of that presentation, Dr. Patel noted that his relatively small but innovative practice has been very successful in the OCM, as measured by CMMI, in reducing costs associated with patient hospitalizations, emergency department visits, and similar metrics, resulting in lower Medicare expenditures per beneficiary, per month. Even very large practices participating in the OCM, such as Florida Cancer Specialists, have seen similar trends in lower hospital utilization and lower overall Medicare treatment costs, as well as reducing drug costs with the increased use of biosimilars. Independent community oncology practices of all sizes, both small to large, urban and rural, have put in a tremendous amount of work with the OCM, even keeping it running during the COVID-19 public health emergency – against all odds, we might add. It is extremely disappointing that CMMI has not done a thorough analysis of what is working in the OCM – and aspects of the OCM have most certainly dramatically improved cancer care while lowering costs – and what is not, building on the successes and correcting the weaknesses.
Some of the answers to questions that CMMI should be seeking include, but are not limited to, the following:
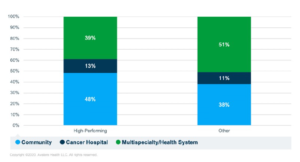
- What is the relative success of independent community oncology practices versus hospital systems in the OCM? Preliminary analysis of OCM performance by Avalere[3] indicates that almost half of “high-performing” practices were independent community oncology practices.
- What have OCM participants that have lowered overall Medicare costs done differently than participants that have not lowered costs? CMMI should be doing an extensive analysis of the OCM that requires time past performance period five, as only then were practices really starting to implement the OCM in full force. Early on in the OCM, we believed that success may have been driven in part due to favorable historical benchmarks. This is supported by an Avalere analysis[1] that “suggests that differences in practice performance may be heavily dependent on expenditure patterns seen prior to the initiation of OCM, thus better positioning some participants for early success.” These are the types of analyses that CMMI should be doing to understand the dynamics of the OCM in refining and making it better, not just trashing it. We know of many community oncology practices that have shown greater success over time as they built on their experience and learnings implementing the OCM during the first few years. We believe that with further analysis of later performance periods, especially focusing on community oncology practices, CMMI will find a marked lowering of costs in the OCM. In fact, we call your attention to CMMI having verbally stated that over half of all OCM participants in performance period eight received a performance-based payment. Results like this should not be ignored and warrant an extension of the OCM for further analysis.
- How has COVID-19 and the public health emergency impacted results? This is a major experimental confounding variable that alone should be reason enough not to summarily discontinue the OCM. Once again, Avalere has analyzed the impact of COVID-19 on the OCM[2], something CMMI should be doing and making available to OCM participants. Avalere found that their analysis “suggests that practices with high rates of beneficiaries being treated for COVID-19 would be least likely to contain expenditure below their target amounts on aggregate, in addition to experiencing care disruptions associated with the response to COVID-19.” We simply can’t understand how CMMI can make any decisions about the OCM in light of the public health emergency still in effect due to COVID-19.
- How has the availability of lower cost biosimilars factored into the OCM results and how can increasing availability be included in an OCM 2.0? We believe that marked uptake of biosimilars by independent community oncology practices positions practices for success in the OCM. Once again, this is the type of analysis CMMI should be doing to refine and enhance the OCM, not summarily abandoning it.
The rumor is that CMMI will not only abandon the OCM but will not be pursuing the successor model, the Oncology Care First (OCF) Model, which CMMI previewed with stakeholders in late 2019. (For reference, we have attached our letter to Director Fowler in response to a request for our input on the OCF concept.)
We also want to address the recent publication in JAMA[3] of the OCM analysis commissioned by CMMI. This analysis, based on only five of the first performance periods is essentially meaningless, for just that reason: The time period measured was the start of the most profound transformation of cancer care ever undertaken. The amount of financial investment, staff education, technology infrastructure build, clinical retooling, etc., was so massive by the most active OCM participants that it would be unrealistic and naïve for CMMI to expect the OCM to produce early positive results, although it did in many cases. We hope that CMMI read the editorial[4] published in JAMA in reaction to the OCM analysis. The authors made so many on-target, insightful comments, and questions, about the analysis that we highlight a few here:
- “In addition, the secular trend of increasing drug prices over the 5 years of the OCM, including use of new, expensive immunotherapies and targeted therapies, constrained the ability of oncologists to make cost-saving therapeutic substitutions.”
- “Moreover, the study examined the first 3 years of the program, which may be too early to realize some benefits. The data show that more practices earned a performance-based payment in period 4, which signals participants’ capacity to reduce costs with time, experience, and performance feedback.”
- “What were the OCM’s spillover effects on non-Medicare patients?”
- “How much additional financial outlays were made by OCM practices in relation to the additional payments received?”
- “How might the presence of multiple different payment models have influenced practice- and clinician-level care experience.”
One of the most on-target observations made by the editorial authors is as follows:
“Furthermore, the inclusion of drug spending in an APM bundle is problematic. Drug costs are increasing steeply as a share of the total cost of cancer care. Including drug spending in a bundle implies that oncologists have discretionary spending power in drug prescribing, which may not be true given the dynamic innovation in cancer treatment. Oncologists will substitute less costly regimens when there is clinical equipoise, such as with biosimilar agents and bone-strengthening agents, but for new agents there are often no viable alternatives. Physicians will be unwilling to make guideline-discordant substitutions that compromise safety or efficacy purely for cost. Drug price negotiation and market-based competition are likely to be more effective policy levers for managing increasing drug spending.”
Finally, in relation to the analysis, we note a fundamental flaw: There is no true “control” group to compare OCM outcomes. CMMI needs to look around at non-OCM independent oncology practices that are participating in commercial models similar to the OCM and innovating both clinical operations and payment design. It’s impossible for CMMI to operate models in a Medicare bubble when the world of medical practice does not, and cannot, silo off Medicare. We fear, this may be a fatal flaw of CMMI ever being successful.
What COA recommends is the following prudent course of action, based in part on the Innovation Center Strategy Refresh, which we believe is investing in the successes of the OCM rather than abandoning it and the learning and totally wasting taxpayers’ money:
- Extend the OCM immediately to, at the very least, December 31, 2022. Ideally, the OCM should be considered a pilot that should be refined over time.
- Convene a roundtable meeting with select OCM participants to discuss what is working with the program and what should be changed. Do what CMMI should be all about – innovate! That comes from understanding both what is working with the OCM and what should be refined, changed, or eliminated.
- COA will work with CMMI in incorporating very specific elements of the Innovation Center Strategy Refresh in the OCM, starting with elements of ensuring health equities in cancer care delivered under the OCM.
- Incorporate a concerted effort on biosimilars utilization into the OCM, including considering waiving patient co-payments on biosimilars. COA is committed to biosimilars, and we believe an OCM 2.0 focused on biosimilar use will dramatically decrease costs.
- Incorporate digital ePRO into the OCM to significantly enhance tracking of patient’s experiences. This is something COA is working on with the Purchaser Business Group on Health.
- Involve not only commercial insurers in the OCM 2.0 but reach out to and involve self-insured employers. Again, innovate!
We ask for a virtual meeting to discuss this letter and our recommendations.
We commend CMMI for the vision of launching the OCM. However, rather than completely abandoning the model, CMMI should be working in concert with stakeholders to advance the model with the goal of enhancing cancer care for Medicare beneficiaries while reducing costs. Our experience with the OCM documents this is achievable. If the current administration is truly committed to “refreshing” the CMMI strategy, CMMI needs to be more collaborative and innovative with stakeholders, starting with those in oncology committed to the OCM.
We would think that given President Biden’s long-standing commitment to the care and cure of cancer, this would be a top priority of his administration. Moreover, we would think that building on the successes in the OCM would be an important step to fulfilling that commitment in terms of enhancing cancer care for all Americans, regardless of socioeconomic status, as we work towards the cure.
We will reach out to schedule a virtual meeting.
Thank you.
Sincerely,
Kashyap Patel, MD Ted Okon
President Executive Director
CC: President Joe Biden
Hon. Richard Neal, Chair, House Committee on Ways and Means
Hon. Frank Pallone, Chair, House Committee on Energy and Commerce
Hon. Ron Wyden, Chair, Senate Committee on Finance
Hon. Kevin Brady, Ranking Member, House Committee on Ways and Means
Hon. Cathy McMorris Rodgers, Ranking Member, House Committee on Energy and Commerce
Hon. Michael Crapo, Ranking Member, Senate Committee on Finance
COA Letter to CMS and CMMI Requesting Extension of OCM
Dear Administrator Brooks-LaSure and Deputy Administrator Fowler:
On behalf of the Board of Directors of the Community Oncology Alliance (“COA”), we are asking you to please extend the Oncology Care Model (“OCM”) past the scheduled termination date of June 30, 2022, and to announce this extension immediately.
As you know, the OCM starts winding down on January 1, 2022, with no new patients enrolled past that date. For important reasons summarized in this letter, the OCM should be extended at least through December 31, 2022, while we commit to working with you and the staff at the Center for Medicare and Medicaid Innovation (“CMMI”) to refine and expand the OCM, with a particular emphasis on correcting health disparities in cancer care. The millions of dollars of taxpayers’ money invested in the OCM and the dramatic successes of many independent community oncology practices participating in the OCM in enhancing patient cancer care while lowering treatment costs, should be clear reasons why the OCM should not be trashed, but refined and re-envisioned based on what is working.
We appreciate your recently announced Innovation Center Strategy Refresh.[1] On paper, many of the “refresh” elements are important facets to making CMMI a success, especially the advancement of health equities, and are pertinent to furthering cancer care in this country; however, the reality faced by community oncology practices is that so many are already deeply invested in the OCM in terms of process change, staff, and infrastructure. In fact, it’s ironic that while the OCM has precipitated the remarkable birth of at least 35 oncology payment reform models in this country[2], with many new novel ones under development, the OCM has apparently been deemed a failure by CMMI after just five performance periods, even though it has been a remarkable success in many independent practices.
Many of the current OCM participants have openly and eagerly shared how the OCM has transformed their practices’ mission, teams, and clinical processes to focus on quality and value in all aspects of the cancer care journey. The OCM was instrumental in creating and fostering that mindset. These practice transformations have led to many new initiatives and arrangements with payers to enhance the quality of cancer care while lowering costs. If the OCM is summarily discontinued, especially without a meaningful next-generation model, the clear message will be delivered that the Centers for Medicare & Medicaid Services (“CMS”) and CMMI have no interest in furthering the transformation of the cancer care delivery system in this country. Significantly, it also forfeits CMMI’s leadership role in innovating oncology payment reform.
Recently, Dr. Kashyap Patel presented to CMMI leadership and staff a successor model to the OCM that would focus specifically on health disparities. During the course of that presentation, Dr. Patel noted that his relatively small but innovative practice has been very successful in the OCM, as measured by CMMI, in reducing costs associated with patient hospitalizations, emergency department visits, and similar metrics, resulting in lower Medicare expenditures per beneficiary, per month. Even very large practices participating in the OCM, such as Florida Cancer Specialists, have seen similar trends in lower hospital utilization and lower overall Medicare treatment costs, as well as reducing drug costs with the increased use of biosimilars. Independent community oncology practices of all sizes, both small to large, urban and rural, have put in a tremendous amount of work with the OCM, even keeping it running during the COVID-19 public health emergency – against all odds, we might add. It is extremely disappointing that CMMI has not done a thorough analysis of what is working in the OCM – and aspects of the OCM have most certainly dramatically improved cancer care while lowering costs – and what is not, building on the successes and correcting the weaknesses.
Some of the answers to questions that CMMI should be seeking include, but are not limited to, the following:
The rumor is that CMMI will not only abandon the OCM but will not be pursuing the successor model, the Oncology Care First (OCF) Model, which CMMI previewed with stakeholders in late 2019. (For reference, we have attached our letter to Director Fowler in response to a request for our input on the OCF concept.)
We also want to address the recent publication in JAMA[3] of the OCM analysis commissioned by CMMI. This analysis, based on only five of the first performance periods is essentially meaningless, for just that reason: The time period measured was the start of the most profound transformation of cancer care ever undertaken. The amount of financial investment, staff education, technology infrastructure build, clinical retooling, etc., was so massive by the most active OCM participants that it would be unrealistic and naïve for CMMI to expect the OCM to produce early positive results, although it did in many cases. We hope that CMMI read the editorial[4] published in JAMA in reaction to the OCM analysis. The authors made so many on-target, insightful comments, and questions, about the analysis that we highlight a few here:
One of the most on-target observations made by the editorial authors is as follows:
“Furthermore, the inclusion of drug spending in an APM bundle is problematic. Drug costs are increasing steeply as a share of the total cost of cancer care. Including drug spending in a bundle implies that oncologists have discretionary spending power in drug prescribing, which may not be true given the dynamic innovation in cancer treatment. Oncologists will substitute less costly regimens when there is clinical equipoise, such as with biosimilar agents and bone-strengthening agents, but for new agents there are often no viable alternatives. Physicians will be unwilling to make guideline-discordant substitutions that compromise safety or efficacy purely for cost. Drug price negotiation and market-based competition are likely to be more effective policy levers for managing increasing drug spending.”
Finally, in relation to the analysis, we note a fundamental flaw: There is no true “control” group to compare OCM outcomes. CMMI needs to look around at non-OCM independent oncology practices that are participating in commercial models similar to the OCM and innovating both clinical operations and payment design. It’s impossible for CMMI to operate models in a Medicare bubble when the world of medical practice does not, and cannot, silo off Medicare. We fear, this may be a fatal flaw of CMMI ever being successful.
What COA recommends is the following prudent course of action, based in part on the Innovation Center Strategy Refresh, which we believe is investing in the successes of the OCM rather than abandoning it and the learning and totally wasting taxpayers’ money:
We ask for a virtual meeting to discuss this letter and our recommendations.
We commend CMMI for the vision of launching the OCM. However, rather than completely abandoning the model, CMMI should be working in concert with stakeholders to advance the model with the goal of enhancing cancer care for Medicare beneficiaries while reducing costs. Our experience with the OCM documents this is achievable. If the current administration is truly committed to “refreshing” the CMMI strategy, CMMI needs to be more collaborative and innovative with stakeholders, starting with those in oncology committed to the OCM.
We would think that given President Biden’s long-standing commitment to the care and cure of cancer, this would be a top priority of his administration. Moreover, we would think that building on the successes in the OCM would be an important step to fulfilling that commitment in terms of enhancing cancer care for all Americans, regardless of socioeconomic status, as we work towards the cure.
We will reach out to schedule a virtual meeting.
Thank you.
Sincerely,
Kashyap Patel, MD Ted Okon
President Executive Director
CC: President Joe Biden
Hon. Richard Neal, Chair, House Committee on Ways and Means
Hon. Frank Pallone, Chair, House Committee on Energy and Commerce
Hon. Ron Wyden, Chair, Senate Committee on Finance
Hon. Kevin Brady, Ranking Member, House Committee on Ways and Means
Hon. Cathy McMorris Rodgers, Ranking Member, House Committee on Energy and Commerce
Hon. Michael Crapo, Ranking Member, Senate Committee on Finance
COA Letter to CMS and CMMI Requesting Extension of OCM
Dear Administrator Brooks-LaSure and Deputy Administrator Fowler:
On behalf of the Board of Directors of the Community Oncology Alliance (“COA”), we are asking you to please extend the Oncology Care Model (“OCM”) past the scheduled termination date of June 30, 2022, and to announce this extension immediately.
As you know, the OCM starts winding down on January 1, 2022, with no new patients enrolled past that date. For important reasons summarized in this letter, the OCM should be extended at least through December 31, 2022, while we commit to working with you and the staff at the Center for Medicare and Medicaid Innovation (“CMMI”) to refine and expand the OCM, with a particular emphasis on correcting health disparities in cancer care. The millions of dollars of taxpayers’ money invested in the OCM and the dramatic successes of many independent community oncology practices participating in the OCM in enhancing patient cancer care while lowering treatment costs, should be clear reasons why the OCM should not be trashed, but refined and re-envisioned based on what is working.
We appreciate your recently announced Innovation Center Strategy Refresh.[1] On paper, many of the “refresh” elements are important facets to making CMMI a success, especially the advancement of health equities, and are pertinent to furthering cancer care in this country; however, the reality faced by community oncology practices is that so many are already deeply invested in the OCM in terms of process change, staff, and infrastructure. In fact, it’s ironic that while the OCM has precipitated the remarkable birth of at least 35 oncology payment reform models in this country[2], with many new novel ones under development, the OCM has apparently been deemed a failure by CMMI after just five performance periods, even though it has been a remarkable success in many independent practices.
Many of the current OCM participants have openly and eagerly shared how the OCM has transformed their practices’ mission, teams, and clinical processes to focus on quality and value in all aspects of the cancer care journey. The OCM was instrumental in creating and fostering that mindset. These practice transformations have led to many new initiatives and arrangements with payers to enhance the quality of cancer care while lowering costs. If the OCM is summarily discontinued, especially without a meaningful next-generation model, the clear message will be delivered that the Centers for Medicare & Medicaid Services (“CMS”) and CMMI have no interest in furthering the transformation of the cancer care delivery system in this country. Significantly, it also forfeits CMMI’s leadership role in innovating oncology payment reform.
Recently, Dr. Kashyap Patel presented to CMMI leadership and staff a successor model to the OCM that would focus specifically on health disparities. During the course of that presentation, Dr. Patel noted that his relatively small but innovative practice has been very successful in the OCM, as measured by CMMI, in reducing costs associated with patient hospitalizations, emergency department visits, and similar metrics, resulting in lower Medicare expenditures per beneficiary, per month. Even very large practices participating in the OCM, such as Florida Cancer Specialists, have seen similar trends in lower hospital utilization and lower overall Medicare treatment costs, as well as reducing drug costs with the increased use of biosimilars. Independent community oncology practices of all sizes, both small to large, urban and rural, have put in a tremendous amount of work with the OCM, even keeping it running during the COVID-19 public health emergency – against all odds, we might add. It is extremely disappointing that CMMI has not done a thorough analysis of what is working in the OCM – and aspects of the OCM have most certainly dramatically improved cancer care while lowering costs – and what is not, building on the successes and correcting the weaknesses.
Some of the answers to questions that CMMI should be seeking include, but are not limited to, the following:
The rumor is that CMMI will not only abandon the OCM but will not be pursuing the successor model, the Oncology Care First (OCF) Model, which CMMI previewed with stakeholders in late 2019. (For reference, we have attached our letter to Director Fowler in response to a request for our input on the OCF concept.)
We also want to address the recent publication in JAMA[3] of the OCM analysis commissioned by CMMI. This analysis, based on only five of the first performance periods is essentially meaningless, for just that reason: The time period measured was the start of the most profound transformation of cancer care ever undertaken. The amount of financial investment, staff education, technology infrastructure build, clinical retooling, etc., was so massive by the most active OCM participants that it would be unrealistic and naïve for CMMI to expect the OCM to produce early positive results, although it did in many cases. We hope that CMMI read the editorial[4] published in JAMA in reaction to the OCM analysis. The authors made so many on-target, insightful comments, and questions, about the analysis that we highlight a few here:
One of the most on-target observations made by the editorial authors is as follows:
“Furthermore, the inclusion of drug spending in an APM bundle is problematic. Drug costs are increasing steeply as a share of the total cost of cancer care. Including drug spending in a bundle implies that oncologists have discretionary spending power in drug prescribing, which may not be true given the dynamic innovation in cancer treatment. Oncologists will substitute less costly regimens when there is clinical equipoise, such as with biosimilar agents and bone-strengthening agents, but for new agents there are often no viable alternatives. Physicians will be unwilling to make guideline-discordant substitutions that compromise safety or efficacy purely for cost. Drug price negotiation and market-based competition are likely to be more effective policy levers for managing increasing drug spending.”
Finally, in relation to the analysis, we note a fundamental flaw: There is no true “control” group to compare OCM outcomes. CMMI needs to look around at non-OCM independent oncology practices that are participating in commercial models similar to the OCM and innovating both clinical operations and payment design. It’s impossible for CMMI to operate models in a Medicare bubble when the world of medical practice does not, and cannot, silo off Medicare. We fear, this may be a fatal flaw of CMMI ever being successful.
What COA recommends is the following prudent course of action, based in part on the Innovation Center Strategy Refresh, which we believe is investing in the successes of the OCM rather than abandoning it and the learning and totally wasting taxpayers’ money:
We ask for a virtual meeting to discuss this letter and our recommendations.
We commend CMMI for the vision of launching the OCM. However, rather than completely abandoning the model, CMMI should be working in concert with stakeholders to advance the model with the goal of enhancing cancer care for Medicare beneficiaries while reducing costs. Our experience with the OCM documents this is achievable. If the current administration is truly committed to “refreshing” the CMMI strategy, CMMI needs to be more collaborative and innovative with stakeholders, starting with those in oncology committed to the OCM.
We would think that given President Biden’s long-standing commitment to the care and cure of cancer, this would be a top priority of his administration. Moreover, we would think that building on the successes in the OCM would be an important step to fulfilling that commitment in terms of enhancing cancer care for all Americans, regardless of socioeconomic status, as we work towards the cure.
We will reach out to schedule a virtual meeting.
Thank you.
Sincerely,
Kashyap Patel, MD Ted Okon
President Executive Director
CC: President Joe Biden
Hon. Richard Neal, Chair, House Committee on Ways and Means
Hon. Frank Pallone, Chair, House Committee on Energy and Commerce
Hon. Ron Wyden, Chair, Senate Committee on Finance
Hon. Kevin Brady, Ranking Member, House Committee on Ways and Means
Hon. Cathy McMorris Rodgers, Ranking Member, House Committee on Energy and Commerce
Hon. Michael Crapo, Ranking Member, Senate Committee on Finance