Community Oncology 2020 Year in Review
While 2020 tested the strength of community oncology, the field thrived in the face of adversity.
Introduction
The Community Oncology Alliance (COA) is continuing its annual tradition of issuing a Year in Review to remember and celebrate the amazing work done by our field in 2020.
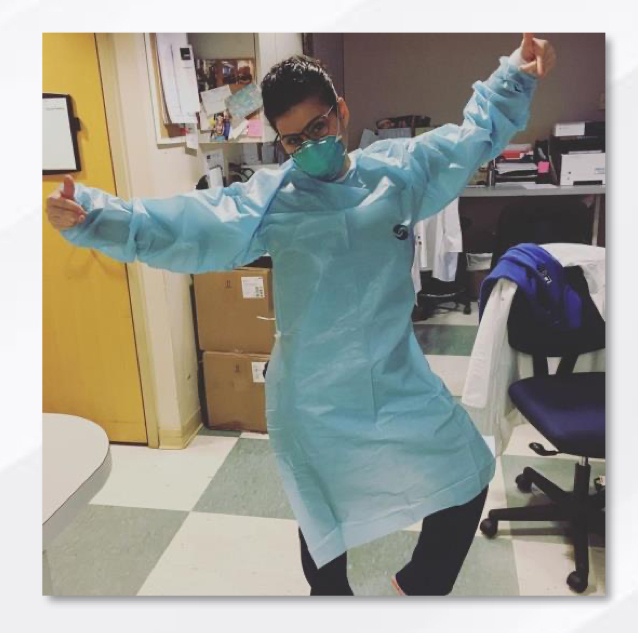
Our community faced a crippling pandemic that challenged patient care, staff, and operations. The field continued to face pressure from hospital consolidations, buyouts, and mergers. Pharmacy Benefit Managers (PBMs) and insurers didn’t stop their relentless, patient unfriendly practices. And new misguided government experiments, like the Radiation Oncology Model and Most Favored Nation model, have threatened to throw the entire cancer care system into disarray.
Community oncology demonstrated that it is resilient, resourceful, and innovative. Practices took on the responsibility of caring for patients when hospitals were (and continue to be) overloaded with COVID-19 patients, providing essential care to some of the nation’s most vulnerable patients by radically altering workflows and stepping up to the plate. Advocates pushed President Trump and Congress to support policies that expanded care access and kept patients safe, and to oppose policies that hurt practices’ ability to provide treatment. Patients thrived because they were able to receive care, despite the pandemic, thanks to the care provided by community oncology.
Introduction cont.
From appealing to the Centers for Medicare & Medicaid Services (CMS) to suspend cumbersome regulatory rules to working with Congress to pass the Coronavirus Aid, Relief, and Economic Security (CARES) Act in March, we’ve been fighting non-stop for the field.
Together, we have met a year’s worth of pandemic challenges and overcome them. 2020 has made it extraordinarily difficult to provide safe, quality cancer care, but you did it. 2021 is shaping up to be a better year, but the specter of COVID-19 still looms. As we cope with the realities of a pandemic and a new presidential administration, new challenges will greet us. COA will support its members as each challenge approaches and pave the way to a better community oncology system. It has been an honor to stand by your side in 2020 and we look forward to standing there in 2021.

Kashyap Patel, MD
President

Michael Diaz, MD
Immediate Past President

Ted Okon, MBA
Executive Director
COA worked with practices, legislators, and regulatory agencies to meet the demands of cancer care and keep patients safe.
Legislative & Regulatory Actions
In previous years, COA has had staff members in D.C. multiple times each month, at least a half-dozen fly-ins, and several advocate Hill Days. While not possible this year, the previous years of investment in relationships with legislators and policy makers has paid off.
COA had a seat at the virtual table, securing several major wins for community oncology in 2020. COA continues to fight for community oncology patients and practices as the year fades into 2021.
When the pandemic began, COA successfully lobbied lawmakers and regulatory bodies to support the nation’s cancer care system. COA was one of the first organizations to push the Department of Health and Human Services (HHS) for provider relief funds and helped practices secure those funds once they were available, saving many practices from closing their doors. The CARES Act, a major piece of COVID-19 relief legislation,
included a suspension of the Medicare reimbursement sequester that we pushed lawmakers to include. If the sequester had remained in effect, many practices would have been pushed beyond the breaking point due to reorganizing around pandemic measures.
Additionally, COA pushed HHS to loosen telehealth regulations during the pandemic. Practices could employ more common teleconferencing software, such as Zoom, to see patients for checkups and some diagnostic visits. These tools kept patients safe at home rather than potentially exposing them to COVID-19. COA continues to advocate for sensible regulation of telehealth tools so community oncology can best serve its patients.
COA also defended cancer care from dangerous PBM actions. In March, COA filed an amicus brief in Rutledge v. Pharmaceutical Care Management Association, a U.S. Supreme Court case that affirmed the right of states to regulate PBMs.
COA had a seat at the virtual table, securing several major wins for community oncology in 2020.

Legislative & Regulatory Actions cont.
PBMs also suggested home infusion of chemotherapy and cancer treatment supportive drugs during the pandemic. These drugs carry a significant risk of adverse reactions, up to and including death. We pushed insurers and regulators to oppose allowing home infusion and put patient safety first.
The Radiation Oncology Model (ROM), originally set to start January 1, 2021, was delayed after an analysis commissioned by COA found that ROM participants were in COVID-19 hotspots, putting physicians and patients in danger by diverting resources away
In 2020, COA made sure community oncology’s voice was heard in Washington.
from prevention and towards the new model. After petitioning HHS, the start date has been pushed back to January 1, 2022, the earliest date it can be implemented. COA continues to monitor the ROM and other developments in the payment reform sphere.
Most recently, President Trump and HHS attempted a last-minute move to implement a mandatory Most Favored Nation (MFN) drug pricing experiment, set to begin on January 1, 2021, that would tie Medicare Part B drug reimbursement to the prices paid in other countries. The MFN experiment would use patients
We issued:
6 Position Statements
12 Comment Letters
23 Press Releases and Media Statements

and practices as pawns to force drug manufacturers to lower prices, and by CMS’ own estimates, nine percent of Medicare seniors would forgo treatment in the first year of the MFN experiment. CMS estimated in two years, a staggering 19 percent, nearly one in five seniors, would not be treated. COA immediately acted, submitting formal comments against the MFN to HHS and suing HHS to stop the MFN experiment, calling it “dangerous and unlawful.” The court issued a preliminary injunction against the MFN experiment pending further review of the case. As of January 11, 2021, the federal government has decided not to challenge the injunction and does not plan to proceed with additional rulemaking.
Patient Advocacy
The pandemic did not slow COA’s advocacy work; advocates stayed busy this year ensuring that patients could get to treatment and afford necessities.
 The country’s economic condition forced closures that hurt patients’ ability to find and receive treatment, and the uncertain status of public transportation made it a no-go for those with vulnerable immune systems. COA partnered with CancerCare, a nonprofit that provides resources to patients with cancer, to create the Patient Assistance Transportation Program and Patient Financial Assistance Fund. The Transportation Program helped patients around the country get to and from treatment in sanitized vehicles at
The country’s economic condition forced closures that hurt patients’ ability to find and receive treatment, and the uncertain status of public transportation made it a no-go for those with vulnerable immune systems. COA partnered with CancerCare, a nonprofit that provides resources to patients with cancer, to create the Patient Assistance Transportation Program and Patient Financial Assistance Fund. The Transportation Program helped patients around the country get to and from treatment in sanitized vehicles at
no cost to the patient, ensuring that needed cancer treatment would continue uninterrupted. For patients experiencing financial hardship due to job loss or other factors, the Financial Assistance Fund provided income that patients could put towards essential items, like food or housing. These initiatives kept patients safe and on track to recovery during the darkest moments of the pandemic.
Additionally, advocates delivered COA and COA Patient Advocacy Network (CPAN) messages on the value of community oncology through the media, supporting the efforts of multiple advocacy organizations, and by sharing their experiences as patients with cancer and survivors. In addition to supporting other advocacy groups,
CPAN served in key opinion leader and speaker roles at multiple national and advocacy oncology events on such diverse topics as community oncology’s role in clinical trials, the impact of COVID-19 on clinical trials, and defining the role and value of advocacy in life science organizations.
Patient Advocacy cont.
CPAN adapted to the pandemic by converting chapter launches to virtual events.
At the very height of the pandemic, CPAN welcomed a new chapter at Genesis Cancer Center in Hot Springs, Arkansas. More virtual launches for 2021 have been scheduled and can be readily converted back to in-person launches pending the end of the pandemic.
The chapters adapted by holding multiple advocacy events each month, beginning the year with in-person meetings and quickly morphing into virtual events as the pandemic flared. Included were such events as Sit in My Chair, a realistic demonstration of the patient experience, with the Deputy Mayor of Syracuse, New York; a Facebook advocacy event in Fort Wayne, Indiana; and a virtual advocacy event in Augusta, Georgia. A re-design of the CPAN website introduced chapter pages highlighting the individual accomplishments of chapters nationwide.
The Advocacy Chat series premiered with monthly webinars featuring policy experts to keep advocates informed. With over 100 attendees per webinar, topics this year included white/brown bagging, end of life care and planning, and more.
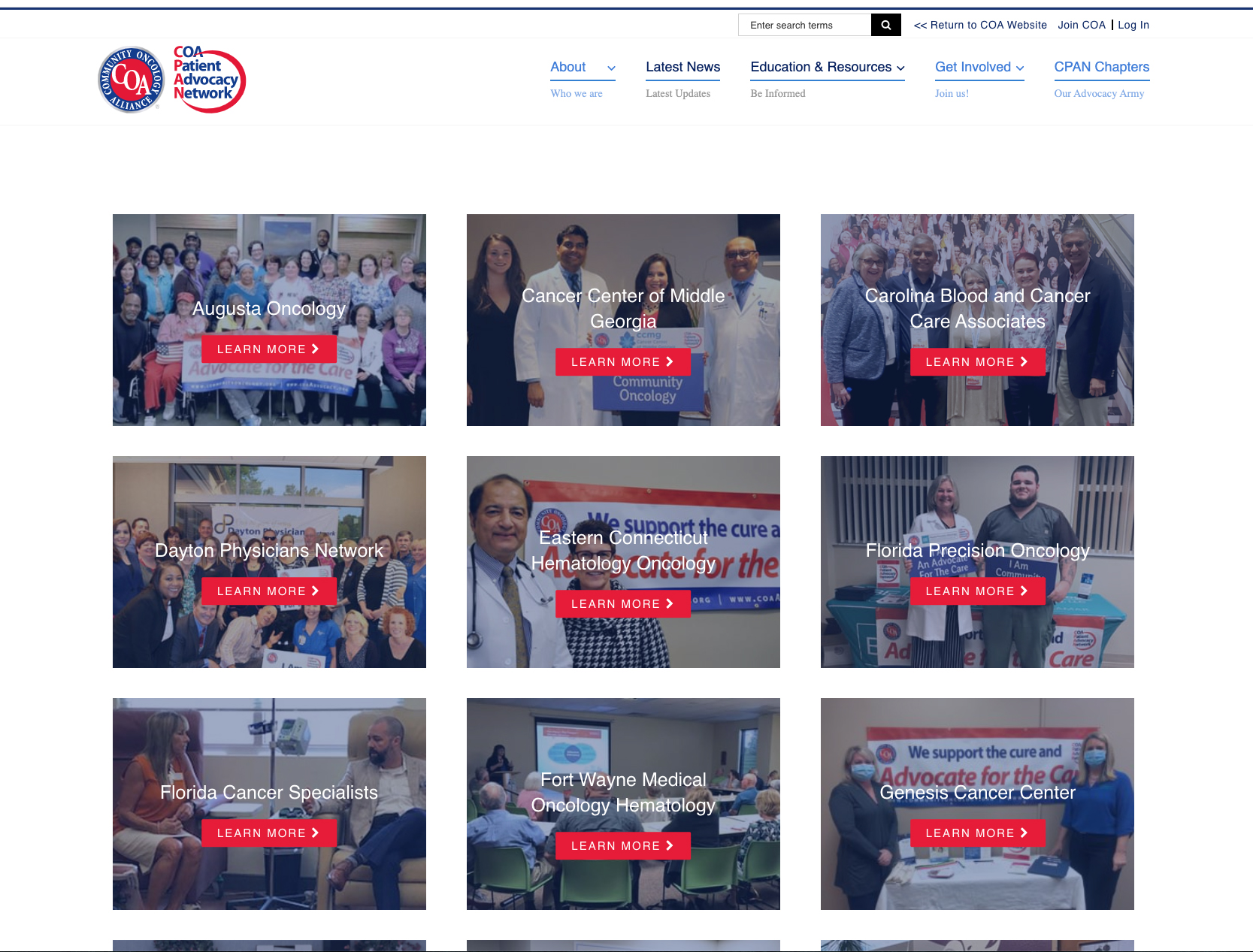
A re-design of the CPAN website introduced chapter pages highlighting the individual accomplishments of chapters nationwide.
Practice Support Resources & Initiatives
Each year, COA creates support tools for physicians, administrators, pharmacists, nurses, nurse assistants, and all other community oncology professionals.
In 2020, these resources focused on COVID-19 relief, but other resources helped practices prepare for 2021 Evaluation and Management (E&M) coding changes, the Oncology Care Model (OCM) 2.0, and holistic practice improvement.
The COA networks stayed busy making sure practices had the latest and greatest information. In November 2019, COA noted the lack of use of newer service codes by cancer practices and a lack of preparation for the 2021 Evaluation and Management coding changes.
 The COA Administrators’ Network (CAN) put together a team of experts to educate oncology practices on the importance of using these new codes. Throughout 2020, the team produced:
The COA Administrators’ Network (CAN) put together a team of experts to educate oncology practices on the importance of using these new codes. Throughout 2020, the team produced:
- An educational workshop to promote new services for patients.
- Ten audiobooks covering the difference between traditional and new billing guidelines.
- Three interactive webinars for administrators and physicians.
- A planning tool for practices to create implementation goals for the new codes.
CAN was also instrumental in securing an extension for the Oncology Care Model, contacting representatives and senators to express concern about switching to the Oncology Care First model during a pandemic.
The COA networks stayed busy making sure practices had the latest and greatest information.
Practice Support Resources & Initiatives cont.
![]() The Community Oncology Pharmacy Association (COPA) worked to support pharmacists as they battled prior authorizations and PBMs in 2020. COPA created resources to help practices streamline appeal processes and get much-needed medications to patients faster.
The Community Oncology Pharmacy Association (COPA) worked to support pharmacists as they battled prior authorizations and PBMs in 2020. COPA created resources to help practices streamline appeal processes and get much-needed medications to patients faster. 
 September 2020 saw the debut of the COA Fellows Educational Institute, a higher education program that teaches oncology and hematology fellows about the value of community oncology. The Institute provides free educational resources to members on major oncology items like the current state of regulation, upcoming reimbursement changes, and more. Currently, 18 institutions, including Johns Hopkins University and Vanderbilt University, have applied to participate in the Fellows Program.
September 2020 saw the debut of the COA Fellows Educational Institute, a higher education program that teaches oncology and hematology fellows about the value of community oncology. The Institute provides free educational resources to members on major oncology items like the current state of regulation, upcoming reimbursement changes, and more. Currently, 18 institutions, including Johns Hopkins University and Vanderbilt University, have applied to participate in the Fellows Program.
![]() COAnalyzer, COA’s free, proprietary benchmarking software for oncology practices, received its biggest update ever in 2020. Users can now view over 850 data elements and compare their performance to competitors by size and location. As practices face pressure from hospitals and government systems, having access to the latest data becomes invaluable.
COAnalyzer, COA’s free, proprietary benchmarking software for oncology practices, received its biggest update ever in 2020. Users can now view over 850 data elements and compare their performance to competitors by size and location. As practices face pressure from hospitals and government systems, having access to the latest data becomes invaluable.
Engaging Employers for the Future of Cancer Care
Employers have long sought solutions that provide high quality care, exceptional patient experience, and affordability. Yet, it has become increasingly difficult to navigate cancer treatment and health care costs continue to rise.
Building on COA’s long history of engaging with employers through events such as the annual Payer Exchange Summit, in 2020, COA launched its most ambitious employer initiative, the National Cancer Treatment Alliance (NCTA).
The NCTA is a new coalition of practices that will engage directly with employers and employer health groups on strategies to reduce costs and improve the quality of cancer care that their employees and others receive. Through educational efforts, data projects, and innovative contracting strategies, NCTA
seeks to fix a system that has been broken by PBMs, insurers, and other middlemen entities that work for themselves instead of the employers that hire them and the patients they affect.
As many cancer drugs are available in oral form and prescription drug benefits are a source of excessive cost and aggravation, the NCTA’s first contracting subsidiary is the Cancer Pharmacy Network (CPN). Functioning as a clinically integrated network, the CPN will provide direct contracting between oncology providers and employers for oral cancer drugs, as well as data-backed informational studies that help shed light and transparency on the opaque world of PBM contracting, rebates, and exclusionary pharmacy networks.

NCTA is changing cancer care by putting employers in direct contact with leading community oncology practices across the country.
Events & Meetings
Using COA’s cutting-edge and interactive virtual events platform, each event brought leading national experts into the homes and offices of community oncologists and other health care professionals throughout the nation.
Annual Conference 2020
The Annual Community Oncology Conference is oncology’s must-attend meeting. Undaunted by a global COVID-19 pandemic, COA rapidly switched from an in-person meeting and opened the 2020 Community Oncology Conference in April as its first completely virtual gathering. More than 4,500 attendees heard from practices on the front lines of the pandemic, researchers exploring new clinical tools to treat cancer, and policy experts with insight on the inner workings of Washington.
Registrants who missed a session or want to review, may access the entire Conference and exhibits on-demand. Log on to www.COAConference.com using your registered email address to access the meeting presentations.

COA took the entire slate of 2020 meetings into the virtual space.
Events & Meetings cont.
2020 Advocacy Summit
In July, CPAN hosted the first ever Community Oncology Advocacy Summit: Cancer Care in a COVID-19 World. More than 800 attendees, including patients, survivors, caregivers, advocates, professionals, and others, heard presentations by national
CPAN hosted the first ever Community Oncology Advocacy Summit.
experts on cancer policy, how cancer treatment has changed due to COVID-19, and new tools, like telehealth, that patients can use to stay safe.
Presentations and recordings of the Advocacy Summit are posted for on-demand viewing by registered attendees.

Payer Exchange Summit
The Payer Exchange Summit on Oncology Payment Reform series is dedicated to advancing payment reform in cancer care. The virtual 2020 Summit held in October was the largest gathering of cancer payment reform stakeholders this year. This invitation-only event featured the most recent advancements and firsthand experiences in oncology payment reform and improving the patient cancer care experience. Attendees left the Summit ready to implement new models at their practices and improve existing ones with the help of new data.

Research & Publications
COA publishes regular reports on critical issues, such as cancer consolidation and payment reform.
We also commission studies that analyze trends on various subjects, like cost of care site differentials, the 340B drug pricing program, PBMs, drug utilization, and the financial impact of sequester cuts. In 2020, COA reviewed the current state of community oncology and payment reform and how the field has been impacted by the pandemic. Each report informs COA’s actions and is used to advance policies beneficial to patients and their care providers.
Practice Impact Report
The 2020 Community Oncology Practice Impact Report tracks the changing landscape of cancer care in the United States. The biennial report is an industry standard on community oncology consolidation. Almost as old as COA itself, the report summarizes the changes that are affecting patient access to local, affordable, quality cancer care. Since 2008, COA has tracked 435 community oncology practices that have closed and 722 community oncology practices that have been acquired or become affiliated with hospitals.
Payment Reform Model Brief
COA released its inaugural Payment Reform Model Brief in 2020. Since 2014, COA has tracked payment reform trends in the U.S. using public and private data. The inaugural brief provides a formal assessment of this data and the current state of payment reform models. According to the report, 35 payment reform models are currently operating in 37 states, with seven models operating in multiple states and four national models.
To read the full brief, visit the Community Oncology Alliance website.
The Impact of COVID-19 on Cancer Care
In 2020, cancer did not stop for COVID-19, but screenings and treatments did. To determine how many patients were foregoing care, COA commissioned a study by Avalere Health that examined the frequencies for common cancer procedures, including screenings, infusion therapies, such as chemotherapy, surgeries, and radiation therapy. Unfortunately, every data point indicated a large drop-off in care. Because of missed screenings and treatment sessions, oncologists expect a surge in diagnoses of later-stage cancers and advanced morbidity in 2021.
The full report is available in JCO Clinical Cancer Informatics.
Community Oncology 2020 Year in Review
While 2020 tested the strength of community oncology, the field thrived in the face of adversity.
Introduction
The Community Oncology Alliance (COA) is continuing its annual tradition of issuing a Year in Review to remember and celebrate the amazing work done by our field in 2020.
Our community faced a crippling pandemic that challenged patient care, staff, and operations. The field continued to face pressure from hospital consolidations, buyouts, and mergers. Pharmacy Benefit Managers (PBMs) and insurers didn’t stop their relentless, patient unfriendly practices. And new misguided government experiments, like the Radiation Oncology Model and Most Favored Nation model, have threatened to throw the entire cancer care system into disarray.
Community oncology demonstrated that it is resilient, resourceful, and innovative. Practices took on the responsibility of caring for patients when hospitals were (and continue to be) overloaded with COVID-19 patients, providing essential care to some of the nation’s most vulnerable patients by radically altering workflows and stepping up to the plate. Advocates pushed President Trump and Congress to support policies that expanded care access and kept patients safe, and to oppose policies that hurt practices’ ability to provide treatment. Patients thrived because they were able to receive care, despite the pandemic, thanks to the care provided by community oncology.
Introduction cont.
From appealing to the Centers for Medicare & Medicaid Services (CMS) to suspend cumbersome regulatory rules to working with Congress to pass the Coronavirus Aid, Relief, and Economic Security (CARES) Act in March, we’ve been fighting non-stop for the field.
Together, we have met a year’s worth of pandemic challenges and overcome them. 2020 has made it extraordinarily difficult to provide safe, quality cancer care, but you did it. 2021 is shaping up to be a better year, but the specter of COVID-19 still looms. As we cope with the realities of a pandemic and a new presidential administration, new challenges will greet us. COA will support its members as each challenge approaches and pave the way to a better community oncology system. It has been an honor to stand by your side in 2020 and we look forward to standing there in 2021.

Kashyap Patel, MD
President

Michael Diaz, MD
Immediate Past President

Ted Okon, MBA
Executive Director
COA worked with practices, legislators, and regulatory agencies to meet the demands of cancer care and keep patients safe.
Legislative & Regulatory Actions
In previous years, COA has had staff members in D.C. multiple times each month, at least a half-dozen fly-ins, and several advocate Hill Days. While not possible this year, the previous years of investment in relationships with legislators and policy makers has paid off.
COA had a seat at the virtual table, securing several major wins for community oncology in 2020. COA continues to fight for community oncology patients and practices as the year fades into 2021.
When the pandemic began, COA successfully lobbied lawmakers and regulatory bodies to support the nation’s cancer care system. COA was one of the first organizations to push the Department of Health and Human Services (HHS) for provider relief funds and helped practices secure those funds once they were available, saving many practices from closing their doors. The CARES Act, a major piece of COVID-19 relief legislation,
included a suspension of the Medicare reimbursement sequester that we pushed lawmakers to include. If the sequester had remained in effect, many practices would have been pushed beyond the breaking point due to reorganizing around pandemic measures.
Additionally, COA pushed HHS to loosen telehealth regulations during the pandemic. Practices could employ more common teleconferencing software, such as Zoom, to see patients for checkups and some diagnostic visits. These tools kept patients safe at home rather than potentially exposing them to COVID-19. COA continues to advocate for sensible regulation of telehealth tools so community oncology can best serve its patients.
COA also defended cancer care from dangerous PBM actions. In March, COA filed an amicus brief in Rutledge v. Pharmaceutical Care Management Association, a U.S. Supreme Court case that affirmed the right of states to regulate PBMs.
COA had a seat at the virtual table, securing several major wins for community oncology in 2020.

Legislative & Regulatory Actions cont.
PBMs also suggested home infusion of chemotherapy and cancer treatment supportive drugs during the pandemic. These drugs carry a significant risk of adverse reactions, up to and including death. We pushed insurers and regulators to oppose allowing home infusion and put patient safety first.
The Radiation Oncology Model (ROM), originally set to start January 1, 2021, was delayed after an analysis commissioned by COA found that ROM participants were in COVID-19 hotspots, putting physicians and patients in danger by diverting resources away
In 2020, COA made sure community oncology’s voice was heard in Washington.
from prevention and towards the new model. After petitioning HHS, the start date has been pushed back to January 1, 2022, the earliest date it can be implemented. COA continues to monitor the ROM and other developments in the payment reform sphere.
Most recently, President Trump and HHS attempted a last-minute move to implement a mandatory Most Favored Nation (MFN) drug pricing experiment, set to begin on January 1, 2021, that would tie Medicare Part B drug reimbursement to the prices paid in other countries. The MFN experiment would use patients
We issued:
6 Position Statements
12 Comment Letters
23 Press Releases and Media Statements

and practices as pawns to force drug manufacturers to lower prices, and by CMS’ own estimates, nine percent of Medicare seniors would forgo treatment in the first year of the MFN experiment. CMS estimated in two years, a staggering 19 percent, nearly one in five seniors, would not be treated. COA immediately acted, submitting formal comments against the MFN to HHS and suing HHS to stop the MFN experiment, calling it “dangerous and unlawful.” The court issued a preliminary injunction against the MFN experiment pending further review of the case. As of January 11, 2021, the federal government has decided not to challenge the injunction and does not plan to proceed with additional rulemaking.
Patient Advocacy
The pandemic did not slow COA’s advocacy work; advocates stayed busy this year ensuring that patients could get to treatment and afford necessities.
 The country’s economic condition forced closures that hurt patients’ ability to find and receive treatment, and the uncertain status of public transportation made it a no-go for those with vulnerable immune systems. COA partnered with CancerCare, a nonprofit that provides resources to patients with cancer, to create the Patient Assistance Transportation Program and Patient Financial Assistance Fund. The Transportation Program helped patients around the country get to and from treatment in sanitized vehicles at
The country’s economic condition forced closures that hurt patients’ ability to find and receive treatment, and the uncertain status of public transportation made it a no-go for those with vulnerable immune systems. COA partnered with CancerCare, a nonprofit that provides resources to patients with cancer, to create the Patient Assistance Transportation Program and Patient Financial Assistance Fund. The Transportation Program helped patients around the country get to and from treatment in sanitized vehicles at
no cost to the patient, ensuring that needed cancer treatment would continue uninterrupted. For patients experiencing financial hardship due to job loss or other factors, the Financial Assistance Fund provided income that patients could put towards essential items, like food or housing. These initiatives kept patients safe and on track to recovery during the darkest moments of the pandemic.
Additionally, advocates delivered COA and COA Patient Advocacy Network (CPAN) messages on the value of community oncology through the media, supporting the efforts of multiple advocacy organizations, and by sharing their experiences as patients with cancer and survivors. In addition to supporting other advocacy groups,
CPAN served in key opinion leader and speaker roles at multiple national and advocacy oncology events on such diverse topics as community oncology’s role in clinical trials, the impact of COVID-19 on clinical trials, and defining the role and value of advocacy in life science organizations.
Patient Advocacy cont.
CPAN adapted to the pandemic by converting chapter launches to virtual events.
At the very height of the pandemic, CPAN welcomed a new chapter at Genesis Cancer Center in Hot Springs, Arkansas. More virtual launches for 2021 have been scheduled and can be readily converted back to in-person launches pending the end of the pandemic.
The chapters adapted by holding multiple advocacy events each month, beginning the year with in-person meetings and quickly morphing into virtual events as the pandemic flared. Included were such events as Sit in My Chair, a realistic demonstration of the patient experience, with the Deputy Mayor of Syracuse, New York; a Facebook advocacy event in Fort Wayne, Indiana; and a virtual advocacy event in Augusta, Georgia. A re-design of the CPAN website introduced chapter pages highlighting the individual accomplishments of chapters nationwide.
The Advocacy Chat series premiered with monthly webinars featuring policy experts to keep advocates informed. With over 100 attendees per webinar, topics this year included white/brown bagging, end of life care and planning, and more.
A re-design of the CPAN website introduced chapter pages highlighting the individual accomplishments of chapters nationwide.
Practice Support Resources & Initiatives
Each year, COA creates support tools for physicians, administrators, pharmacists, nurses, nurse assistants, and all other community oncology professionals.
In 2020, these resources focused on COVID-19 relief, but other resources helped practices prepare for 2021 Evaluation and Management (E&M) coding changes, the Oncology Care Model (OCM) 2.0, and holistic practice improvement.
The COA networks stayed busy making sure practices had the latest and greatest information. In November 2019, COA noted the lack of use of newer service codes by cancer practices and a lack of preparation for the 2021 Evaluation and Management coding changes.
 The COA Administrators’ Network (CAN) put together a team of experts to educate oncology practices on the importance of using these new codes. Throughout 2020, the team produced:
The COA Administrators’ Network (CAN) put together a team of experts to educate oncology practices on the importance of using these new codes. Throughout 2020, the team produced:
- An educational workshop to promote new services for patients.
- Ten audiobooks covering the difference between traditional and new billing guidelines.
- Three interactive webinars for administrators and physicians.
- A planning tool for practices to create implementation goals for the new codes.
CAN was also instrumental in securing an extension for the Oncology Care Model, contacting representatives and senators to express concern about switching to the Oncology Care First model during a pandemic.
The COA networks stayed busy making sure practices had the latest and greatest information.
Practice Support Resources & Initiatives cont.
![]() The Community Oncology Pharmacy Association (COPA) worked to support pharmacists as they battled prior authorizations and PBMs in 2020. COPA created resources to help practices streamline appeal processes and get much-needed medications to patients faster.
The Community Oncology Pharmacy Association (COPA) worked to support pharmacists as they battled prior authorizations and PBMs in 2020. COPA created resources to help practices streamline appeal processes and get much-needed medications to patients faster. 
 September 2020 saw the debut of the COA Fellows Educational Institute, a higher education program that teaches oncology and hematology fellows about the value of community oncology. The Institute provides free educational resources to members on major oncology items like the current state of regulation, upcoming reimbursement changes, and more. Currently, 18 institutions, including Johns Hopkins University and Vanderbilt University, have applied to participate in the Fellows Program.
September 2020 saw the debut of the COA Fellows Educational Institute, a higher education program that teaches oncology and hematology fellows about the value of community oncology. The Institute provides free educational resources to members on major oncology items like the current state of regulation, upcoming reimbursement changes, and more. Currently, 18 institutions, including Johns Hopkins University and Vanderbilt University, have applied to participate in the Fellows Program.
![]() COAnalyzer, COA’s free, proprietary benchmarking software for oncology practices, received its biggest update ever in 2020. Users can now view over 850 data elements and compare their performance to competitors by size and location. As practices face pressure from hospitals and government systems, having access to the latest data becomes invaluable.
COAnalyzer, COA’s free, proprietary benchmarking software for oncology practices, received its biggest update ever in 2020. Users can now view over 850 data elements and compare their performance to competitors by size and location. As practices face pressure from hospitals and government systems, having access to the latest data becomes invaluable.
Engaging Employers for the Future of Cancer Care
Employers have long sought solutions that provide high quality care, exceptional patient experience, and affordability. Yet, it has become increasingly difficult to navigate cancer treatment and health care costs continue to rise.
Building on COA’s long history of engaging with employers through events such as the annual Payer Exchange Summit, in 2020, COA launched its most ambitious employer initiative, the National Cancer Treatment Alliance (NCTA).
The NCTA is a new coalition of practices that will engage directly with employers and employer health groups on strategies to reduce costs and improve the quality of cancer care that their employees and others receive. Through educational efforts, data projects, and innovative contracting strategies, NCTA
seeks to fix a system that has been broken by PBMs, insurers, and other middlemen entities that work for themselves instead of the employers that hire them and the patients they affect.
As many cancer drugs are available in oral form and prescription drug benefits are a source of excessive cost and aggravation, the NCTA’s first contracting subsidiary is the Cancer Pharmacy Network (CPN). Functioning as a clinically integrated network, the CPN will provide direct contracting between oncology providers and employers for oral cancer drugs, as well as data-backed informational studies that help shed light and transparency on the opaque world of PBM contracting, rebates, and exclusionary pharmacy networks.

NCTA is changing cancer care by putting employers in direct contact with leading community oncology practices across the country.
Events & Meetings
Using COA’s cutting-edge and interactive virtual events platform, each event brought leading national experts into the homes and offices of community oncologists and other health care professionals throughout the nation.
Annual Conference 2020
The Annual Community Oncology Conference is oncology’s must-attend meeting. Undaunted by a global COVID-19 pandemic, COA rapidly switched from an in-person meeting and opened the 2020 Community Oncology Conference in April as its first completely virtual gathering. More than 4,500 attendees heard from practices on the front lines of the pandemic, researchers exploring new clinical tools to treat cancer, and policy experts with insight on the inner workings of Washington.
Registrants who missed a session or want to review, may access the entire Conference and exhibits on-demand. Log on to www.COAConference.com using your registered email address to access the meeting presentations.

COA took the entire slate of 2020 meetings into the virtual space.
Events & Meetings cont.
2020 Advocacy Summit
In July, CPAN hosted the first ever Community Oncology Advocacy Summit: Cancer Care in a COVID-19 World. More than 800 attendees, including patients, survivors, caregivers, advocates, professionals, and others, heard presentations by national
CPAN hosted the first ever Community Oncology Advocacy Summit.
experts on cancer policy, how cancer treatment has changed due to COVID-19, and new tools, like telehealth, that patients can use to stay safe.
Presentations and recordings of the Advocacy Summit are posted for on-demand viewing by registered attendees.

Payer Exchange Summit
The Payer Exchange Summit on Oncology Payment Reform series is dedicated to advancing payment reform in cancer care. The virtual 2020 Summit held in October was the largest gathering of cancer payment reform stakeholders this year. This invitation-only event featured the most recent advancements and firsthand experiences in oncology payment reform and improving the patient cancer care experience. Attendees left the Summit ready to implement new models at their practices and improve existing ones with the help of new data.

Research & Publications
COA publishes regular reports on critical issues, such as cancer consolidation and payment reform.
We also commission studies that analyze trends on various subjects, like cost of care site differentials, the 340B drug pricing program, PBMs, drug utilization, and the financial impact of sequester cuts. In 2020, COA reviewed the current state of community oncology and payment reform and how the field has been impacted by the pandemic. Each report informs COA’s actions and is used to advance policies beneficial to patients and their care providers.
Practice Impact Report
The 2020 Community Oncology Practice Impact Report tracks the changing landscape of cancer care in the United States. The biennial report is an industry standard on community oncology consolidation. Almost as old as COA itself, the report summarizes the changes that are affecting patient access to local, affordable, quality cancer care. Since 2008, COA has tracked 435 community oncology practices that have closed and 722 community oncology practices that have been acquired or become affiliated with hospitals.
Payment Reform Model Brief
COA released its inaugural Payment Reform Model Brief in 2020. Since 2014, COA has tracked payment reform trends in the U.S. using public and private data. The inaugural brief provides a formal assessment of this data and the current state of payment reform models. According to the report, 35 payment reform models are currently operating in 37 states, with seven models operating in multiple states and four national models.
To read the full brief, visit the Community Oncology Alliance website.
The Impact of COVID-19 on Cancer Care
In 2020, cancer did not stop for COVID-19, but screenings and treatments did. To determine how many patients were foregoing care, COA commissioned a study by Avalere Health that examined the frequencies for common cancer procedures, including screenings, infusion therapies, such as chemotherapy, surgeries, and radiation therapy. Unfortunately, every data point indicated a large drop-off in care. Because of missed screenings and treatment sessions, oncologists expect a surge in diagnoses of later-stage cancers and advanced morbidity in 2021.
The full report is available in JCO Clinical Cancer Informatics.