2020 Mid-Year Member Update
Introduction
Dear COA Members and Supporters,
2020 has not been the year many expected it would be. Although predictions of jetpacks and cities on the moon were discarded long ago, many saw 2020 as a fresh start to a new decade. Instead, the COVID-19 (novel coronavirus) pandemic has caused upheaval among community oncology patients and practices, requiring everyone to quickly adapt to a new normal.
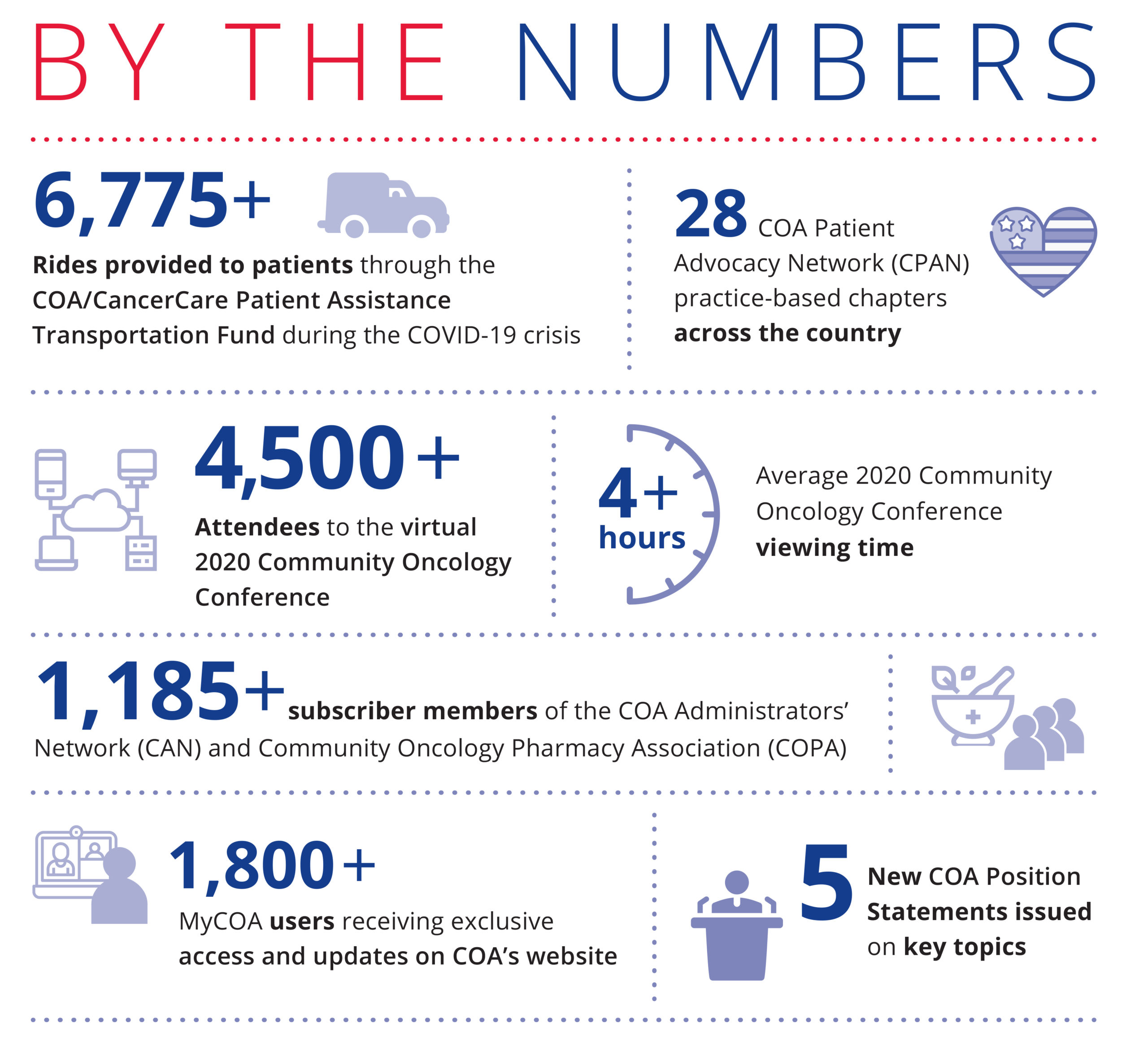
The Community Oncology Alliance (COA) quickly rose to the challenge of supporting patients and practices nationwide, shifting focus where needed and launching several new initiatives you will read about in this update. This Mid-Year Update shares some of the more important updates and work COA has undertaken so far in 2020 for our patients, community oncology practice members, and supporters.
Over the last few months, COA has kept up the pressure on policymakers on Capitol Hill. We worked closely with the Centers for Medicare and Medicaid Services (CMS) to successfully loosen telehealth regulations during the pandemic and urged them to do away with dangerous prior authorization policies. We have fought, and continue to fight, the dangerous proposal of home infusion that could harm or kill patients. To help practices survive so they could stay open to treat patients, we pushed the Administration and Congress for financial relief, including relief payments and stopping the Medicare sequester cut under the CARES Act. Although we are not walking the halls in Washington, we continue to advocate for community oncology and talk daily to the decision makers in Congress, the White House, and key federal agencies.
These days the role of community oncology is as important as ever, but the stakes are higher for patients and providers. COA’s support for you does not waver. We are working every day to protect, maintain, and expand the critically important role community oncology plays in caring for more than half of our country’s patients with cancer.

Supporting Practices and Patients During the COVID-19 Pandemic
The COVID-19 pandemic has obviously hit patients and practices hard, and from the beginning, COA moved in swiftly to launch support efforts to mitigate the impact and danger of this devastating virus. Given the seriousness of patient care during the pandemic, COA took a generous step by making COVID-19 support available well beyond COA members to anyone affected, including health departments, hospitals, other specialties, and stakeholders.
COA worked day and night to ensure that any COVID-19 relief passed in Washington included community oncology practices. A major win was the CARES Act suspension of the sequester cut to Medicare reimbursement from May to December 2020 for all providers, which we fought hard for.
As HHS and Congress began efforts to provide financial relief to providers, COA provided in-depth support to practices on accessing pandemic Relief Funds and Paycheck Protection Program (PPP) loans, including guidelines on how to apply and compliance issues to watch out for.
COA immediately launched a dedicated COVID-19 email listserv. This was the first time practices could “talk” in a private, online format about this rapidly developing situation. Practices were able to ask questions, exchange resources, and tell others about coding, billing, or patient care techniques. The “have you ever” and “I just learned” emails allow members to learn from and teach each other. Today, almost 480 health care workers are part of the COVID-19 listserv.
In addition to the listserv, COA set up the “COVID-19 Practice Resources and Protocols” page on our website. This page hosts the latest information from the federal government on clinical, billing, and administrative information,
and allows practices to share proprietary tools with other practices to fight this pandemic.
As the situation evolved and new policies and practices emerged, COA hosted two webinars to assist practices with prepping and adapting for COVID-19. The first was a general assessment of the impact of COVID-19 on practices, with testimonies from three practices in pandemic hotspots. The second focused on telehealth. COA secured two CMS representatives to present, answer questions, and offer practices guidance during the webinar. The webinar also featured the setup and execution of telehealth systems by four sample practices.
For patients who have faced financial hardships and care disruption as hospital-based centers stopped treatments to handle pandemic patients, COA created the Patient Practice Connector, a free program to ensure patients could find accessible treatment in their area. We also partnered with CancerCare to start the Patient Assistance Transportation Program and Patient Financial Assistance Fund. The Patient Assistance Transportation Program is free for patients and practices, and helps patients get to and from treatment in fully sanitized vehicles. The Patient Financial Assistance Fund provides grants of $500 to help patients with living, transportation, and treatment-related expenses.

Tracking a Changing Independent Practice Landscape with the 2020 COA Practice Impact Report
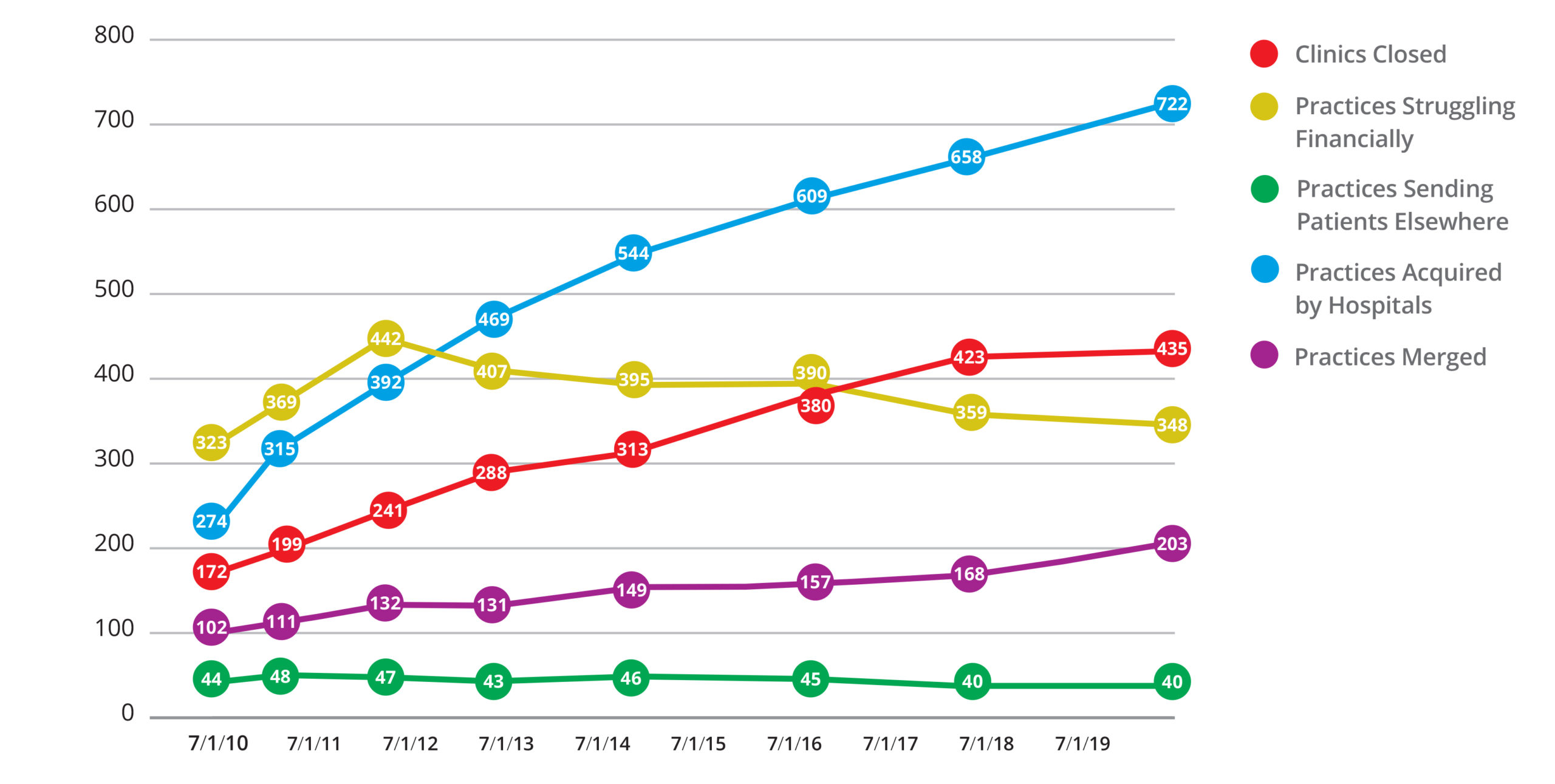
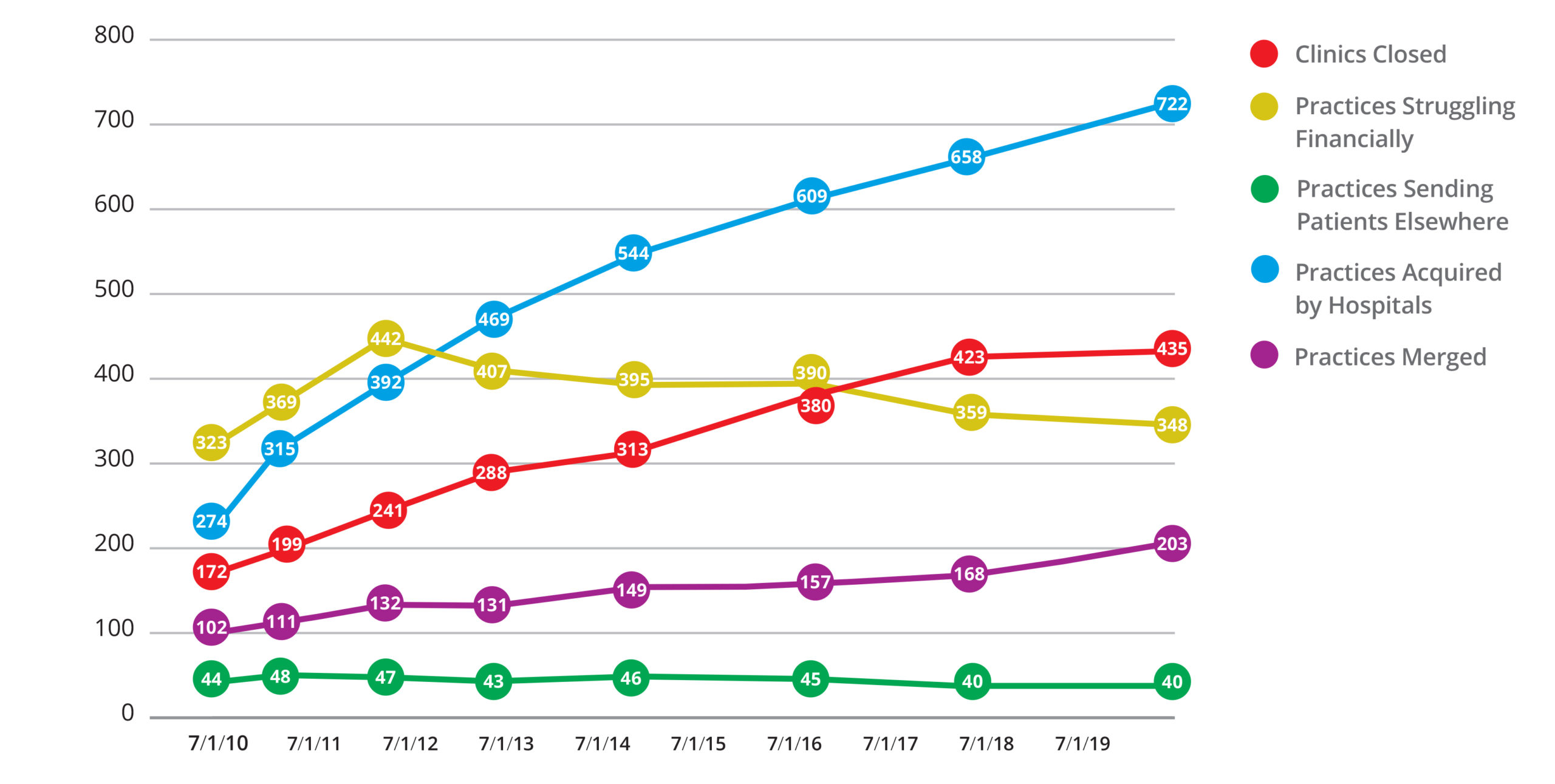
Since COA first introduced the Practice Impact Report in 2008, it has become the industry standard on the state of community oncology. It provides a look at the real numbers behind the pressures on community oncology as practices care for their patients in the face of consolidation, the predatory tactics of pharmacy benefit managers (PBMs), and the unfair pricing advantages of the 340B Drug Pricing Program for hospitals and their contracted pharmacies.
Released during our annual Community Oncology Conference, the 2020 COA Practice Impact Report is our eighth update. It shows that over the last 12 years, 1,748 community oncology clinics and/or practices have closed, been acquired by hospitals, undergone corporate mergers, or reported that they are struggling financially.
The biggest highlight is that since the last report in 2018, there has been a 20.8 percent increase in practices merging with, or being acquired by, another community oncology
practice and/or acquired by a corporate entity. This major jump is likely the result of practices seeking protection from hospital merger pressures. The rate of practice acquisition by hospitals continued at a steady pace, with a 9.7 percent increase from 2018 to 2020 fueled most notably by hospitals’ financial incentives in the 340B Drug Pricing Program and higher payments to hospitals for cancer care services.
The full 2020 COA Practice Impact Report is available here.

Oncology Payment Reform Continues to Move Forward Through the OCM, OCM 2.0, and OCF
The current oncology reimbursement system is not sustainable for patients, providers, or payors and must change. COA has long been the leader in efforts to reform the way cancer care is paid for, delivered, and experienced by patients. We serve as the voice for independent practices as new models and pilot programs are put forth.
The most substantial oncology payment reform model today remains the federal Oncology Care Model (OCM), but on the horizon are its named successor, the Oncology Care First (OCF) model, as well as COA’s proposed Oncology Care Model 2.0 (OCM 2.0).
Oncology Care Model (OCM)
We continue our efforts to help practices succeed and thrive in the OCM through the interactive OCM Support Network, which includes regular calls and meetings, a dedicated listserv, access to subject matter experts, and more. The Network has been a rousing success, with 80 percent of all OCM practices having participated since day one. Earlier this year, when CMS raised the issue of two-sided risk, COA surveyed the practices participating in the OCM and determined that 69 percent wanted to remain in the program with two-sided risk. COA continues to offer support to all practices in anticipation of the presumed mandatory conversion to a two-sided risk format as fee-for-service reimbursement fades. COVID-19 has disrupted practices’ ability to participate in the OCM and continue any gains seen, so COA successfully petitioned the Centers for Medicare and Medicaid Innovation (CMMI) to extend the OCM through 2021.
Oncology Care First (OCF) model
At the first mention of OCF as a potential successor to OCM in late 2019, COA issued comments on the OCF model Request for Information (RFI) and appealed to CMS on behalf of all practices to adopt a more feasible transition period and to extend OCM for one more year. COA further suggested five areas within the RFI that are of concern and offered methodology recommendations on each to improve OCF and benefit patients and participating practices.
OCM 2.0
As a longtime thought leader in oncology payment reform, COA has been listening and learning from the current OCM to understand and plan. The result is a new framework of guidelines for evolving the program so that momentum is not lost, and value-based oncology care can succeed — not just for Medicare or Medicaid, but for commercial payors and employers as well. Known as OCM 2.0, this universal model borrows and builds upon the OCM to provide a fundamental structure for the future of oncology payment reform, including payment for drugs. So far this year we have continued development of a full and detailed OCM 2.0 model for practices and payers, details of which were discussed at the 2020 Community Oncology Conference (recordings are available online) and will continue to be showcased at our upcoming Payer Exchange Summit.

Driving Change with Employers and Purchasers:
The National Cancer Treatment Alliance (NCTA)
COA launched a major new organization, the National Cancer Treatment Alliance (NCTA), earlier this spring to help employers understand and navigate the increasingly complex world of cancer care for their own employees.
 Employers, who are often self-insured, are becoming more aware of the power and important role they can play in ensuring the health care they pay for is both high-value and patient-friendly. Instead of rubberstamping foolhardy practices such as prior authorization, they can instead disrupt the convoluted cancer care delivery system.
Employers, who are often self-insured, are becoming more aware of the power and important role they can play in ensuring the health care they pay for is both high-value and patient-friendly. Instead of rubberstamping foolhardy practices such as prior authorization, they can instead disrupt the convoluted cancer care delivery system.
NCTA’s initial work will be focused on providing fundamental education and actionable guidance to employers on key cancer care issues. It will also develop programs for employers on topics in oncology, such as:
- Optimizing cancer screening and prevention
- Understanding biosimilars and maximizing their use
- How to navigate molecular diagnostic testing
- Understanding immunotherapy and “precision medicine”
- Navigating the opaque PBM rebate trap
The NCTA’s ultimate goal is to contract directly with employers for cancer drugs and services so that their employees have access to the highest-quality, most affordable, and locally accessible cancer care. As many cancer drugs are available in oral form, NCTA is developing its first contracting subsidiary, the Cancer Pharmacy Network (CPN). CPN will function as a clinically integrated network providing direct contracting for oral cancer drugs between oncology providers and employers, as well as data-backed informational studies that help shed light and transparency on the opaque world of PBM contracting, rebates, and exclusionary pharmacy networks. Stay tuned for more from the NCTA!

A Virtual Success:
Bringing the Community Together for the 2020 Community Oncology Conference
The 2020 Community Oncology Conference was like no other in the history of COA. COVID-19 forced a switch from an in-person to virtual conference, giving COA the opportunity to bring this amazing Conference directly to attendees’ homes or offices.
Nationally recognized experts spoke on topics that directly affect community oncology practices and patients every day — the OCM, clinical trials, telehealth, pharmacy benefit managers (PBMs), and much more. Attendees from across the country were able to take the knowledge they gained back to their practices. Going virtual meant compressing the agenda from four tracks to two. Always the most encompassing Conference of the year, nearly 4,500 people attended the Conference (almost three times more than previous years). The Exhibit Hall, where some of the newest treatments and advances in cancer care were featured, had more than 25,000 visits! Overall viewing time was a phenomenal average of 4 hours and 16 minutes.
Taking full advantage of the ability to go virtual to offer education and engagement to wider audiences, COA continued its success with a dedicated virtual Patient Advocacy Summit on July 15, 2020. The virtual Advocacy Summit provided timely updates on key issues impacting cancer care in America today and education on how patients, survivors, caregivers — our most important voices in advocacy — and others can be stronger advocates for the care they want and deserve.
Recordings from both the 2020 Community Oncology Conference and the Patient Advocacy Summit are available for on-demand watching on the COA website at https://communityoncology.org/meetings/.
Please note that you must have been registered for these events in order to view the presentations.


New Position Statements:
Taking a Stand on Key Issues
As the trusted voice of community oncology on policy issues in Washington, D.C., COA has continued to speak out on the key initiatives facing our members and secured community oncology’s seat at the table.
In the first half of 2020, the COA Board of Directors and Government Affairs and Policy Committee issued five formal Position Statements. These statements addressed Home Infusion, Sequestra-tion Cuts, Copay Accumulators, Prior Authoriza-tion, and Certificate of Need (CON) Requirements, and join our growing library of 13 official COA Position Statements on major issues.
Home Infusion: Community oncology practices are taking drastic measures to protect patients during the COVID-19 pandemic. However, COA opposes one of the proposed measures, the home infusion of chemotherapy, cancer immunotherapy, and cancer treatment supportive drugs. These drugs can carry significant risk and should be administered by a trained oncology professional in a setting where the patient can be monitored for adverse reactions.
Sequestration Cuts: COA believes that the sequestration cuts contained within the Budget Control Act of 2011 have been applied inappropriately. The Act mandated a two percent sequestration cut to the Medicare drug reimbursement formula. Rather than apply the two percent cut to the six percent add-on section of the formula, CMS has applied the cut to the Average Sales Price plus the six percent add-on. COA opposes this application and has filed a lawsuit in the U.S. District Court for the District of Columbia to stop it.
Copay Accumulators: COA opposes the use of copay accumulator programs by PBMs. Normal copay assistance programs help patients afford the cost of expensive cancer drugs and
allow the full cost paid by the patient and the program combined to count toward the patient’s deductible. Under copay accumulators, only the portion paid by the patient counts towards the deductible. This increases out-of-pocket costs for patients and causes many to avoid treatment, increasing the likelihood of harm or death. Accumulators are yet another example of PBMs putting profit over human lives.
Prior Authorization: Prior authorization is a cost-control process implemented by health insurance companies to reduce cost and fraud by restricting access to a prescribed treatment, test, or medical service until a physician obtains payor approval. Failure to obtain prior approval might mean a procedure does not qualify for payment. Although the desire to control these elements is understandable, the current appeals process for prior authorization is cumbersome and can result in life-threatening treatment delays. COA suggests eliminating “fail-first” therapies for metastatic cancers, not requiring prior authorization for physicians who meet certain benchmarks, and other guidelines to fix this broken system.
Certificate of Need (CON) Requirements: A CON is an endorsement that many states require before approving the construction of a new health care facility. The central assertion of CON legislation is that overbuilding and redun-dancy in health care facilities leads to higher health care costs. COA opposes CONs on the grounds that they restrict access to treatment by creating provider scarcity in certain areas, increase travel time to appointments, and impose other burdens on patients’ health.

Providing Ongoing Support to People and Practices in the Community Through CAN, CPAN, and COPA
Since our earliest days, COA has run several standing networks that are dedicated to supporting every individual within and that relies upon community oncology. These organizations address the specific issues related to practice administration and operations, in-house pharmacies, and advocacy. The first half of 2020 has reaffirmed the necessity of these groups as practices had to quickly adapt to a new normal of telehealth, social distancing, and more, learning along the way. Through it all, the COA networks were there to support them!
COA Administrators’ Network (CAN)
CAN remains focused on increasing practice operation efficiencies and providing a unified advocacy voice with both Medicare and public
payors. So far this year, CAN members have discussed how they are dealing with the predatory financial practices of PBMs. COA, at the urging of CAN members, submitted a request to CMMI to extend OCM by one year. CMMI agreed to the extension. Another critical assist to CAN members has been the integration of telehealth into practice operations to establish a working telehealth program. As early as April, many CAN member practices were able to successfully add telehealth services to better serve patients during the COVID-19 pandemic.
In addition to regular, monthly meetings, CAN hosted two webinars to assist practices with prepping and adapting for COVID-19. The first was a general assessment of the impact of COVID-19 on practices, with testimonies from three practices in pandemic hotspots. The second focused on telehealth. COA secured two CMS representatives to present, answer questions, and offer practices guidance
Community Oncology Pharmacy Association (COPA)
COPA is expanding and offering more tools for the community oncology pharmacist. In 2020, COPA has grown to almost 800 members who are using these tools and networking with each other to the benefit of their practices. COPA continues to lead the fight with PBMs on behalf of all of community oncology. COPA has surveyed member practices about their experiences with PBMs and is producing a white paper that will examine the most frequent and egregious PBM tactics such as limiting access, slow rolling applications, white bagging, and under reimbursement.
during the webinar. The webinar also featured the setup and execution of telehealth systems to four sample practices.
COA Patient Advocacy Network (CPAN)
CPAN advocates — including patients, survivors, caregivers, nurses, pharmacists, oncologists, and more — share their personal stories and advocacy power so elected officials understand the importance of local, affordable, and accessible cancer care. COVID-19 has limited the opportunity for CPAN members to branch out into their communities; however, CPAN is ready to launch six new chapters as soon as travel and meeting restrictions are loosened. Despite the quarantine rules, CPAN chapters have hosted 11 advocacy events. Every CPAN chapter is also preparing to hold signature “Sit in My Chair” briefings for legislators and staff when they are in-district in August and can tour practices. During these valuable visits, practices provide an important perspective on issues and advocate for changes.
COAnalyzer
COAnalyzer is a completely free benchmarking tool for managing oncology practices. It allows practices to maximize operations with real-time data on how they are performing and how this compares to peers, including benchmarks. Provided free of charge to all COA members, COAnalyzer allows a practice to access over 850 data elements that yield both charts and graphs to illustrate a practice’s comparative performance against their region and similar practices. In 2020, over 100 practices are using the program.
Together We Are Community Strong
In 2020, COA continues to be the representative voice of community oncology. COA offers members unsurpassed benefits and differentiated content, all with the goal of preserving continued access to local, affordable, quality care for patients with cancer.
As the voice of community oncology with policymakers, COA has a leading role in crafting the policies and legislation affecting practices. In addition to our unparalleled support programs for community oncology professionals, no other organization brings you more ways for your practice to connect with the people and resources you need to help you be successful.
As we enter the second half of 2020 and beyond, COA is there for patients and practices. We look forward to creating a safe, secure environment for community oncology to thrive so physicians can deliver effective, affordable care to their communities.
Community Oncology Alliance
1225 New York Ave. NW, Suite 600, Washington, DC 20005
Telephone (202) 729-8147 | info@COAcancer.org | www.communityoncology.org
2020 Mid-Year Member Update
Introduction
Dear COA Members and Supporters,
2020 has not been the year many expected it would be. Although predictions of jetpacks and cities on the moon were discarded long ago, many saw 2020 as a fresh start to a new decade. Instead, the COVID-19 (novel coronavirus) pandemic has caused upheaval among community oncology patients and practices, requiring everyone to quickly adapt to a new normal.
The Community Oncology Alliance (COA) quickly rose to the challenge of supporting patients and practices nationwide, shifting focus where needed and launching several new initiatives you will read about in this update. This Mid-Year Update shares some of the more important updates and work COA has undertaken so far in 2020 for our patients, community oncology practice members, and supporters.
Over the last few months, COA has kept up the pressure on policymakers on Capitol Hill. We worked closely with the Centers for Medicare and Medicaid Services (CMS) to successfully loosen telehealth regulations during the pandemic and urged them to do away with dangerous prior authorization policies. We have fought, and continue to fight, the dangerous proposal of home infusion that could harm or kill patients. To help practices survive so they could stay open to treat patients, we pushed the Administration and Congress for financial relief, including relief payments and stopping the Medicare sequester cut under the CARES Act. Although we are not walking the halls in Washington, we continue to advocate for community oncology and talk daily to the decision makers in Congress, the White House, and key federal agencies.
These days the role of community oncology is as important as ever, but the stakes are higher for patients and providers. COA’s support for you does not waver. We are working every day to protect, maintain, and expand the critically important role community oncology plays in caring for more than half of our country’s patients with cancer.

Supporting Practices and Patients During the COVID-19 Pandemic
The COVID-19 pandemic has obviously hit patients and practices hard, and from the beginning, COA moved in swiftly to launch support efforts to mitigate the impact and danger of this devastating virus. Given the seriousness of patient care during the pandemic, COA took a generous step by making COVID-19 support available well beyond COA members to anyone affected, including health departments, hospitals, other specialties, and stakeholders.
COA worked day and night to ensure that any COVID-19 relief passed in Washington included community oncology practices. A major win was the CARES Act suspension of the sequester cut to Medicare reimbursement from May to December 2020 for all providers, which we fought hard for.
As HHS and Congress began efforts to provide financial relief to providers, COA provided in-depth support to practices on accessing pandemic Relief Funds and Paycheck Protection Program (PPP) loans, including guidelines on how to apply and compliance issues to watch out for.
COA immediately launched a dedicated COVID-19 email listserv. This was the first time practices could “talk” in a private, online format about this rapidly developing situation. Practices were able to ask questions, exchange resources, and tell others about coding, billing, or patient care techniques. The “have you ever” and “I just learned” emails allow members to learn from and teach each other. Today, almost 480 health care workers are part of the COVID-19 listserv.
In addition to the listserv, COA set up the “COVID-19 Practice Resources and Protocols” page on our website. This page hosts the latest information from the federal government on clinical, billing, and administrative information,
and allows practices to share proprietary tools with other practices to fight this pandemic.
As the situation evolved and new policies and practices emerged, COA hosted two webinars to assist practices with prepping and adapting for COVID-19. The first was a general assessment of the impact of COVID-19 on practices, with testimonies from three practices in pandemic hotspots. The second focused on telehealth. COA secured two CMS representatives to present, answer questions, and offer practices guidance during the webinar. The webinar also featured the setup and execution of telehealth systems by four sample practices.
For patients who have faced financial hardships and care disruption as hospital-based centers stopped treatments to handle pandemic patients, COA created the Patient Practice Connector, a free program to ensure patients could find accessible treatment in their area. We also partnered with CancerCare to start the Patient Assistance Transportation Program and Patient Financial Assistance Fund. The Patient Assistance Transportation Program is free for patients and practices, and helps patients get to and from treatment in fully sanitized vehicles. The Patient Financial Assistance Fund provides grants of $500 to help patients with living, transportation, and treatment-related expenses.

Tracking a Changing Independent Practice Landscape with the 2020 COA Practice Impact Report
Since COA first introduced the Practice Impact Report in 2008, it has become the industry standard on the state of community oncology. It provides a look at the real numbers behind the pressures on community oncology as practices care for their patients in the face of consolidation, the predatory tactics of pharmacy benefit managers (PBMs), and the unfair pricing advantages of the 340B Drug Pricing Program for hospitals and their contracted pharmacies.
Released during our annual Community Oncology Conference, the 2020 COA Practice Impact Report is our eighth update. It shows that over the last 12 years, 1,748 community oncology clinics and/or practices have closed, been acquired by hospitals, undergone corporate mergers, or reported that they are struggling financially.
The biggest highlight is that since the last report in 2018, there has been a 20.8 percent increase in practices merging with, or being acquired by, another community oncology
practice and/or acquired by a corporate entity. This major jump is likely the result of practices seeking protection from hospital merger pressures. The rate of practice acquisition by hospitals continued at a steady pace, with a 9.7 percent increase from 2018 to 2020 fueled most notably by hospitals’ financial incentives in the 340B Drug Pricing Program and higher payments to hospitals for cancer care services.
The full 2020 COA Practice Impact Report is available here.

Oncology Payment Reform Continues to Move Forward Through the OCM, OCM 2.0, and OCF
The current oncology reimbursement system is not sustainable for patients, providers, or payors and must change. COA has long been the leader in efforts to reform the way cancer care is paid for, delivered, and experienced by patients. We serve as the voice for independent practices as new models and pilot programs are put forth.
The most substantial oncology payment reform model today remains the federal Oncology Care Model (OCM), but on the horizon are its named successor, the Oncology Care First (OCF) model, as well as COA’s proposed Oncology Care Model 2.0 (OCM 2.0).
Oncology Care Model (OCM)
We continue our efforts to help practices succeed and thrive in the OCM through the interactive OCM Support Network, which includes regular calls and meetings, a dedicated listserv, access to subject matter experts, and more. The Network has been a rousing success, with 80 percent of all OCM practices having participated since day one. Earlier this year, when CMS raised the issue of two-sided risk, COA surveyed the practices participating in the OCM and determined that 69 percent wanted to remain in the program with two-sided risk. COA continues to offer support to all practices in anticipation of the presumed mandatory conversion to a two-sided risk format as fee-for-service reimbursement fades. COVID-19 has disrupted practices’ ability to participate in the OCM and continue any gains seen, so COA successfully petitioned the Centers for Medicare and Medicaid Innovation (CMMI) to extend the OCM through 2021.
Oncology Care First (OCF) model
At the first mention of OCF as a potential successor to OCM in late 2019, COA issued comments on the OCF model Request for Information (RFI) and appealed to CMS on behalf of all practices to adopt a more feasible transition period and to extend OCM for one more year. COA further suggested five areas within the RFI that are of concern and offered methodology recommendations on each to improve OCF and benefit patients and participating practices.
OCM 2.0
As a longtime thought leader in oncology payment reform, COA has been listening and learning from the current OCM to understand and plan. The result is a new framework of guidelines for evolving the program so that momentum is not lost, and value-based oncology care can succeed — not just for Medicare or Medicaid, but for commercial payors and employers as well. Known as OCM 2.0, this universal model borrows and builds upon the OCM to provide a fundamental structure for the future of oncology payment reform, including payment for drugs. So far this year we have continued development of a full and detailed OCM 2.0 model for practices and payers, details of which were discussed at the 2020 Community Oncology Conference (recordings are available online) and will continue to be showcased at our upcoming Payer Exchange Summit.

Driving Change with Employers and Purchasers:
The National Cancer Treatment Alliance (NCTA)
COA launched a major new organization, the National Cancer Treatment Alliance (NCTA), earlier this spring to help employers understand and navigate the increasingly complex world of cancer care for their own employees.
 Employers, who are often self-insured, are becoming more aware of the power and important role they can play in ensuring the health care they pay for is both high-value and patient-friendly. Instead of rubberstamping foolhardy practices such as prior authorization, they can instead disrupt the convoluted cancer care delivery system.
Employers, who are often self-insured, are becoming more aware of the power and important role they can play in ensuring the health care they pay for is both high-value and patient-friendly. Instead of rubberstamping foolhardy practices such as prior authorization, they can instead disrupt the convoluted cancer care delivery system.
NCTA’s initial work will be focused on providing fundamental education and actionable guidance to employers on key cancer care issues. It will also develop programs for employers on topics in oncology, such as:
- Optimizing cancer screening and prevention
- Understanding biosimilars and maximizing their use
- How to navigate molecular diagnostic testing
- Understanding immunotherapy and “precision medicine”
- Navigating the opaque PBM rebate trap
The NCTA’s ultimate goal is to contract directly with employers for cancer drugs and services so that their employees have access to the highest-quality, most affordable, and locally accessible cancer care. As many cancer drugs are available in oral form, NCTA is developing its first contracting subsidiary, the Cancer Pharmacy Network (CPN). CPN will function as a clinically integrated network providing direct contracting for oral cancer drugs between oncology providers and employers, as well as data-backed informational studies that help shed light and transparency on the opaque world of PBM contracting, rebates, and exclusionary pharmacy networks. Stay tuned for more from the NCTA!

A Virtual Success:
Bringing the Community Together for the 2020 Community Oncology Conference
The 2020 Community Oncology Conference was like no other in the history of COA. COVID-19 forced a switch from an in-person to virtual conference, giving COA the opportunity to bring this amazing Conference directly to attendees’ homes or offices.
Nationally recognized experts spoke on topics that directly affect community oncology practices and patients every day — the OCM, clinical trials, telehealth, pharmacy benefit managers (PBMs), and much more. Attendees from across the country were able to take the knowledge they gained back to their practices. Going virtual meant compressing the agenda from four tracks to two. Always the most encompassing Conference of the year, nearly 4,500 people attended the Conference (almost three times more than previous years). The Exhibit Hall, where some of the newest treatments and advances in cancer care were featured, had more than 25,000 visits! Overall viewing time was a phenomenal average of 4 hours and 16 minutes.
Taking full advantage of the ability to go virtual to offer education and engagement to wider audiences, COA continued its success with a dedicated virtual Patient Advocacy Summit on July 15, 2020. The virtual Advocacy Summit provided timely updates on key issues impacting cancer care in America today and education on how patients, survivors, caregivers — our most important voices in advocacy — and others can be stronger advocates for the care they want and deserve.
Recordings from both the 2020 Community Oncology Conference and the Patient Advocacy Summit are available for on-demand watching on the COA website at https://communityoncology.org/meetings/.
Please note that you must have been registered for these events in order to view the presentations.


New Position Statements:
Taking a Stand on Key Issues
As the trusted voice of community oncology on policy issues in Washington, D.C., COA has continued to speak out on the key initiatives facing our members and secured community oncology’s seat at the table.
In the first half of 2020, the COA Board of Directors and Government Affairs and Policy Committee issued five formal Position Statements. These statements addressed Home Infusion, Sequestra-tion Cuts, Copay Accumulators, Prior Authoriza-tion, and Certificate of Need (CON) Requirements, and join our growing library of 13 official COA Position Statements on major issues.
Home Infusion: Community oncology practices are taking drastic measures to protect patients during the COVID-19 pandemic. However, COA opposes one of the proposed measures, the home infusion of chemotherapy, cancer immunotherapy, and cancer treatment supportive drugs. These drugs can carry significant risk and should be administered by a trained oncology professional in a setting where the patient can be monitored for adverse reactions.
Sequestration Cuts: COA believes that the sequestration cuts contained within the Budget Control Act of 2011 have been applied inappropriately. The Act mandated a two percent sequestration cut to the Medicare drug reimbursement formula. Rather than apply the two percent cut to the six percent add-on section of the formula, CMS has applied the cut to the Average Sales Price plus the six percent add-on. COA opposes this application and has filed a lawsuit in the U.S. District Court for the District of Columbia to stop it.
Copay Accumulators: COA opposes the use of copay accumulator programs by PBMs. Normal copay assistance programs help patients afford the cost of expensive cancer drugs and
allow the full cost paid by the patient and the program combined to count toward the patient’s deductible. Under copay accumulators, only the portion paid by the patient counts towards the deductible. This increases out-of-pocket costs for patients and causes many to avoid treatment, increasing the likelihood of harm or death. Accumulators are yet another example of PBMs putting profit over human lives.
Prior Authorization: Prior authorization is a cost-control process implemented by health insurance companies to reduce cost and fraud by restricting access to a prescribed treatment, test, or medical service until a physician obtains payor approval. Failure to obtain prior approval might mean a procedure does not qualify for payment. Although the desire to control these elements is understandable, the current appeals process for prior authorization is cumbersome and can result in life-threatening treatment delays. COA suggests eliminating “fail-first” therapies for metastatic cancers, not requiring prior authorization for physicians who meet certain benchmarks, and other guidelines to fix this broken system.
Certificate of Need (CON) Requirements: A CON is an endorsement that many states require before approving the construction of a new health care facility. The central assertion of CON legislation is that overbuilding and redun-dancy in health care facilities leads to higher health care costs. COA opposes CONs on the grounds that they restrict access to treatment by creating provider scarcity in certain areas, increase travel time to appointments, and impose other burdens on patients’ health.

Providing Ongoing Support to People and Practices in the Community Through CAN, CPAN, and COPA
Since our earliest days, COA has run several standing networks that are dedicated to supporting every individual within and that relies upon community oncology. These organizations address the specific issues related to practice administration and operations, in-house pharmacies, and advocacy. The first half of 2020 has reaffirmed the necessity of these groups as practices had to quickly adapt to a new normal of telehealth, social distancing, and more, learning along the way. Through it all, the COA networks were there to support them!
COA Administrators’ Network (CAN)
CAN remains focused on increasing practice operation efficiencies and providing a unified advocacy voice with both Medicare and public
payors. So far this year, CAN members have discussed how they are dealing with the predatory financial practices of PBMs. COA, at the urging of CAN members, submitted a request to CMMI to extend OCM by one year. CMMI agreed to the extension. Another critical assist to CAN members has been the integration of telehealth into practice operations to establish a working telehealth program. As early as April, many CAN member practices were able to successfully add telehealth services to better serve patients during the COVID-19 pandemic.
In addition to regular, monthly meetings, CAN hosted two webinars to assist practices with prepping and adapting for COVID-19. The first was a general assessment of the impact of COVID-19 on practices, with testimonies from three practices in pandemic hotspots. The second focused on telehealth. COA secured two CMS representatives to present, answer questions, and offer practices guidance
Community Oncology Pharmacy Association (COPA)
COPA is expanding and offering more tools for the community oncology pharmacist. In 2020, COPA has grown to almost 800 members who are using these tools and networking with each other to the benefit of their practices. COPA continues to lead the fight with PBMs on behalf of all of community oncology. COPA has surveyed member practices about their experiences with PBMs and is producing a white paper that will examine the most frequent and egregious PBM tactics such as limiting access, slow rolling applications, white bagging, and under reimbursement.
during the webinar. The webinar also featured the setup and execution of telehealth systems to four sample practices.
COA Patient Advocacy Network (CPAN)
CPAN advocates — including patients, survivors, caregivers, nurses, pharmacists, oncologists, and more — share their personal stories and advocacy power so elected officials understand the importance of local, affordable, and accessible cancer care. COVID-19 has limited the opportunity for CPAN members to branch out into their communities; however, CPAN is ready to launch six new chapters as soon as travel and meeting restrictions are loosened. Despite the quarantine rules, CPAN chapters have hosted 11 advocacy events. Every CPAN chapter is also preparing to hold signature “Sit in My Chair” briefings for legislators and staff when they are in-district in August and can tour practices. During these valuable visits, practices provide an important perspective on issues and advocate for changes.
COAnalyzer
COAnalyzer is a completely free benchmarking tool for managing oncology practices. It allows practices to maximize operations with real-time data on how they are performing and how this compares to peers, including benchmarks. Provided free of charge to all COA members, COAnalyzer allows a practice to access over 850 data elements that yield both charts and graphs to illustrate a practice’s comparative performance against their region and similar practices. In 2020, over 100 practices are using the program.
Together We Are Community Strong
In 2020, COA continues to be the representative voice of community oncology. COA offers members unsurpassed benefits and differentiated content, all with the goal of preserving continued access to local, affordable, quality care for patients with cancer.
As the voice of community oncology with policymakers, COA has a leading role in crafting the policies and legislation affecting practices. In addition to our unparalleled support programs for community oncology professionals, no other organization brings you more ways for your practice to connect with the people and resources you need to help you be successful.
As we enter the second half of 2020 and beyond, COA is there for patients and practices. We look forward to creating a safe, secure environment for community oncology to thrive so physicians can deliver effective, affordable care to their communities.
Community Oncology Alliance
1225 New York Ave. NW, Suite 600, Washington, DC 20005
Telephone (202) 729-8147 | info@COAcancer.org | www.communityoncology.org